CHICAGO, Ill. — COVID-19 can trigger a host of different side-effects in patients. Since the start of the pandemic, doctors have reported seeing patients with swelling of the fingers and toes to even more extreme cases such as hearing loss. Now, a new study is confirming that the virus is causing the body’s own immune system to attack itself. Researchers from Northwestern University say this is resulting in “long lasting and even bizarre” symptoms that may last for the rest of the patient’s life.
The study notes most people who contract COVID suffer only mild symptoms such as muscle soreness and achy joints. For some patients however, these symptoms are more severe and include rheumatoid arthritis flares and autoimmune myositis — or “COVID toes.”
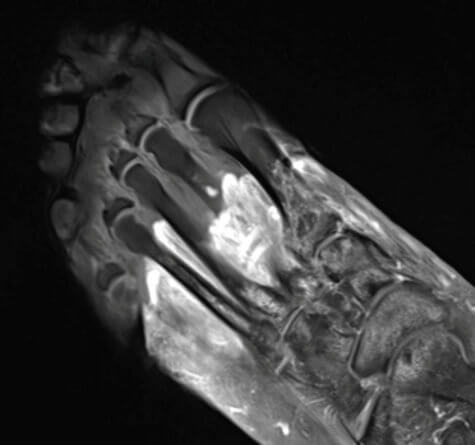
Despite scientists working around the clock to unravel the mysteries of COVID-19, doctors have struggled to explain exactly what causes these long-term symptoms. Using radiological images, the Northwestern team believes they have identified the culprit, the patient’s own immune system.
“We’ve realized that the COVID virus can trigger the body to attack itself in different ways, which may lead to rheumatological issues that require lifelong management,” study author Dr. Swati Deshmukh says in a media release.
‘More insidious’ than the flu
Researchers analyzed data from patients visiting Northwestern Memorial Hospital between May 2020 and December 2020. Some of the patients with long-lasting symptoms received an MRI, CT scan, or ultrasound during their hospitalization. Looking at these images, the researchers determined the origin and nature of their symptoms.
“Many patients with COVID-related musculoskeletal disorders recover, but for some individuals, their symptoms become serious, are deeply concerning to the patient or impact their quality of life, which leads them to seek medical attention and imaging,” Dr. Deshmukh explains.
“That imaging allows us to see if COVID-related muscle and joint pain, for example, are not just body aches similar to what we see from the flu — but something more insidious.”
The scans revealed inflammation, damaged nerves, and blood clots caused by the body’s immune system in response to the virus.
“We might see edema and inflammatory changes of the tissues (fluid, swelling), hematomas (collections of blood) or devitalized tissue (gangrene),” Deshmukh adds. “In some patients, the nerves are injured (bright, enlarged) and in others, the problem is impaired blood flow (clots).”
Body scans may reveal COVID before other symptoms appear
Study authors say, in previous cases, doctors could not put their finger on what was wrong because they did not know what to look for.

“Some doctors request imaging for patients with ‘COVID toes,’ for example, but there wasn’t any literature on imaging of foot and soft tissue complications of COVID,” the corresponding author says. “How do you find something if you’re unsure of what to look for? So in our paper, we discuss the various types of musculoskeletal abnormalities that radiologists should look for and provide imaging examples.”
Radiological imaging, like MRI or CT scans, could help doctors point patients in the right direction when it comes to treatment. Deshmukh recommends that if a patient has persistent shoulder pain starting after they contracted COVID, their primary care doctor should order an MRI or ultrasound.
If radiologists know coronavirus can trigger inflammatory arthritis and the images reveal joint inflammation, COVID patients can quickly get to a rheumatologist for further evaluation. Study authors say radiologists may even be able to suggest a COVID diagnosis by looking at musculoskeletal imaging in patients who didn’t know they contracted the virus.
The findings appear in the journal Skeletal Radiology.
SWNS writer Tom Campbell contributed to this report.
