ANN ARBOR, Mich. — Long after recovery, many Americans are still rife with a different kind of pain: financial stress. Researchers from the University of Michigan are showing just how devastating a hospital stay can be for the average American nowadays. Their study reveals that incidents of both medical debt entering the collections process and bankruptcy are much higher among working-age Americans following hospitalization for traumatic injury.
Study authors report the percentage of Americans with medical debts so overdue that a collection agency gets involved, as well as the size of those debts, tends to be much higher among those who suffered an injury serious enough to require a hospital stay over the prior two years. Those who had recently been hospitalized were also about twice as likely to declare bankruptcy.
The research team compared two groups of Americans between the ages of 18 and 65. Both had the same kind of commercial health insurance but suffered major injuries in different years.
Participants whose major injuries took place in 18 months before study authors took a “snapshot” of their finances were 23 percent more likely to have medical bills in debt collections. Similarly, this group also had 70 percent larger amounts of medical debt in collections. Few individuals across both groups filed for bankruptcy, but such an action was twice as common among those hospitalized for a traumatic injury over the past year-and-a-half.
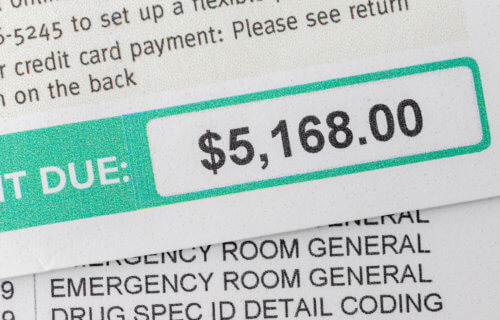
Patients end up owing thousands in out-of-pocket expenses
According to first study author John Scott, M.D., M.P.H., this work highlights the urgent need to restructure health insurance plans and reduce or cap cost-sharing for highly necessary trauma care. Dr. Scott is an assistant professor of surgery, and cares for critically injured patients at Michigan Medicine, U-M’s academic medical center.
“Much of our medical research to date has focused on improving outcomes while patients are in the hospital, but our understanding of the way patients’ lives are affected as they recover has always been limited,” Scott says in a university release. “Our findings show that the negative impact of traumatic injuries on patients’ lives does not end when they leave the hospital. Instead, they have bills that they cannot pay, and there is emerging evidence this debt may further impact their ability to achieve an optimal recovery.”
In collaboration with Nora Becker, M.D., Ph.D., an assistant professor of internal medicine, and others from the Michigan Health Economics and Affordability Lab (M-HEAL), Dr. Scott linked the insurance records from nearly 5,400 people to their credit reports from January 2021. Importantly, the records were anonymous to protect the identities of those involved.
Researchers were sure to choose participants hospitalized in 2019 and early 2020 (the “post-injury” credit data group). They also recruited others who were similar in many ways except that their hospitalization occurred later on in 2021 (the “pre-injury” credit data group). Patients across both groups spent an average of five days in the hospital, including at least one night in the intensive care unit for just over a third of both groups.
Depending on each patient’s health insurance plan, these individuals may have had to deal with out-of-pocket co-pays and deductibles worth hundreds or thousands of dollars for inpatient care and follow-up appointments, study authors note.
Why do insurance plans do this?
Insurers and employers typically use deductibles and co-pays to drive down unnecessary use of health care, but these aren’t “optional” visits to the hospital. Study authors stress that post-injury care is largely not discretionary – it’s necessary for survival and positive long-term health outcomes.
“No one is overconsuming trauma care just because their deductible is low,” Dr. Scott concludes. “Eliminating or capping deductibles for traumatic injuries – just like the recent policies capping the cost of insulin for Medicare patients — could go a long way to ensure that all patients can achieve an optimal recovery after injury. If we fail to acknowledge the reality of the economic challenges our patients really face, then we risk curing patients into destitution.”
The study is published in JAMA Health Forum.