SHANGHAI, China — A tiny implant has cured mice of breast cancer in just two weeks, according to a new study. The self-charging battery enables a new class of medications to kill tumors, leaving healthy tissue alone.
Scientists in China explain that the device runs on salt water injected into the cancerous area, causing consumption of oxygen. Cancer cells starve without the gas, a condition called hypoxia. The technique boosts efficiency of HAPs (hypoxia-activated prodrugs) that seek to exploit this trait by only killing hypoxic cells.
“After 14 days, the tumors in the five mice that received both the working battery and HAP treatment had decreased by an average of 90 percent – with four of these mice experiencing complete tumor disappearance,” says lead author Professor Fan Zhang from Fudan University, according to a report in New Scientist, per SWNS.
“Conversely, the tumors in the other mice groups either remained the same size or increased.”
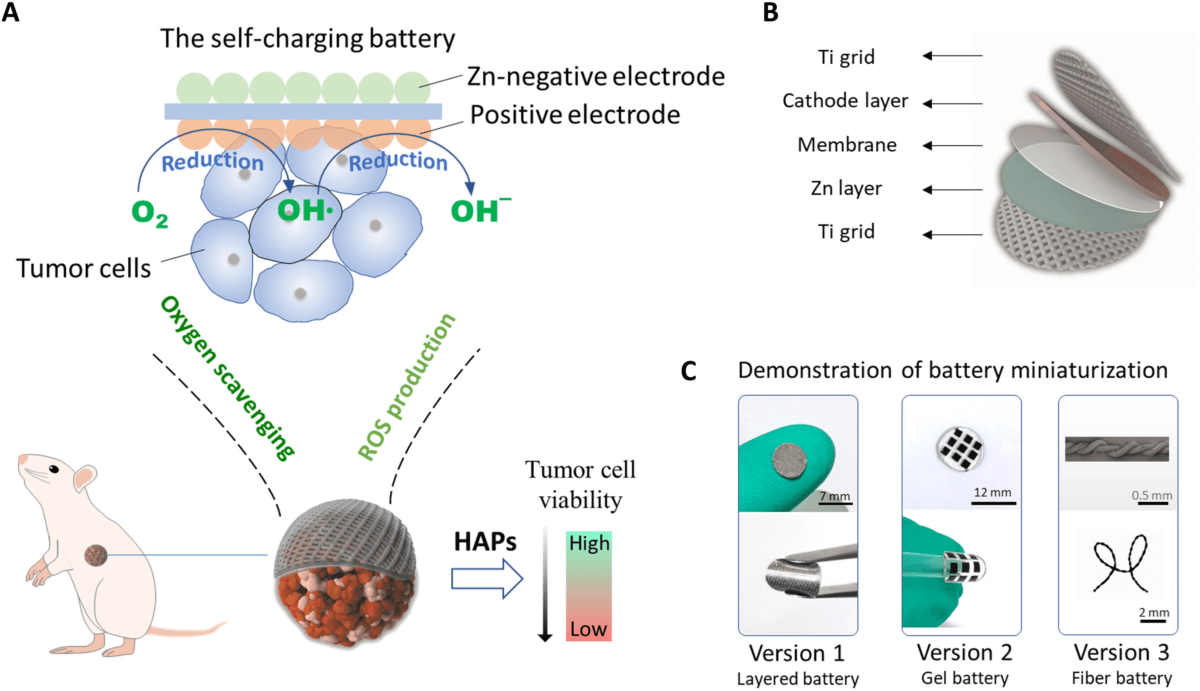
The Chinese team placed the device inside the armpits of 25 lab rodents with breast cancer. Study authors split the other rodents into groups that received no treatment, HAP drugs only, a non-functional implanted battery, or just the working battery.
The implant can operate for up to 500 hours within mouse tissue, producing very low voltage electricity. The idea is to optimize the action of the drugs by creating a hypoxic environment.
HAPs are not currently approved for clinical use due to limited evidence of their effectiveness.
“Tumors typically deplete the oxygen in the surrounding non-cancerous tissues as they grow, resulting in the cells becoming oxygen-free, or hypoxic,” Prof. Zhang explains.
“Hypoxia-activated prodrugs aim to take advantage of this feature by only targeting hypoxic cells – minimizing damage to healthy cells and reducing side effects.”
“The battery can cover the tumor and persistently consume the oxygen within it for more than 14 days, which is much longer than previous agents that worked for usually not more than two days.”
Prof. Randall Johnson of Cambridge University says inducing hypoxia in a tumor can increase the risk the cancer will spread.
“While this didn’t appear to occur in these mice, the costs and benefits of the battery’s use in people needs to be assessed before any human treatment,” Prof. Johnson concludes.
The American Cancer Society estimates that there will be 297,790 new cases of invasive breast cancer in women throughout the United States in 2023.
The study is published in the journal Science Advances.
South West News Service writer Mark Waghorn contributed to this report.

The costs need to be assessed.
If it doesn’t cost much, it will disappear.