BOSTON — Call it the Captain America of medications. An antibiotic from the 1940s could make a stunning comeback to save the world from deadly bacterial strains. This 80-year-old medicine was previously discarded by scientists, but a new study finds it may offer protection against antibiotic-resistant superbugs. These germs can lead to hard-to-treat and potentially fatal infections, according to researchers from Harvard Medical School.
Nourseothricin, a natural product produced by a soil fungus, comprises several variations of a complex molecule called streptothricin. Its discovery in the 1940s incited optimism for its potential as a potent weapon against gram-negative bacteria, which are particularly difficult to eliminate with other antibiotics due to their robust protective outer layer. However, nourseothricin was found to be harmful to human kidneys, resulting in the discontinuation of its development.
Nevertheless, the emergence of antibiotic-resistant bacterial infections has necessitated the search for new medications. This led James Kirby, a pathology professor at Harvard Medical School, and his colleagues to revisit nourseothricin. He believes that earlier studies of nourseothricin suffered from insufficient purification of the streptothricins.
Recent research has revealed that the various forms of streptothricin have different levels of toxicity. One form, streptothricin-F, is significantly less toxic while remaining highly effective against current multidrug-resistant pathogens.
Scroll down to see 3 ways people can encounter antibiotic-resistant bacteria
The research team examined the antibacterial action, kidney toxicity, and mechanism of action of highly purified forms of two different streptothricins, D and F. The professor stated that the D form was more potent than the F form against drug-resistant Enterobacterales and other bacterial species, but it also induced kidney toxicity at a lower dose.
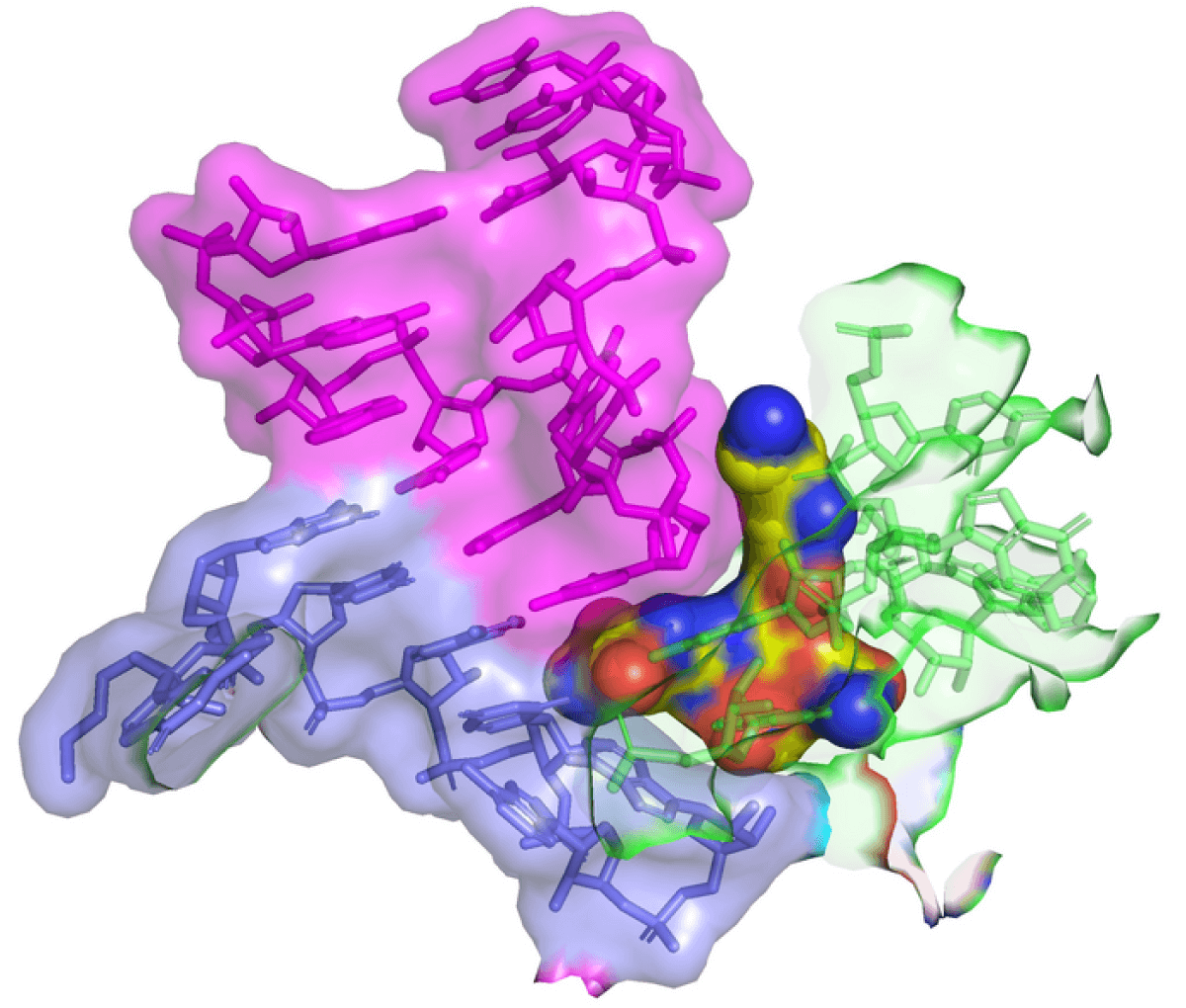
Employing advanced cryo-electron microscopy, the research team demonstrated that streptothricin-F extensively binds to a subunit of the bacterial ribosome. This finding explains the translation errors these antibiotics are known to induce in their target bacteria.
“Based on unique, promising activity, we believe the streptothricin scaffold deserves further pre-clinical exploration as a potential therapeutic for the treatment of multidrug-resistant, Gram-negative pathogens,” says Kirby in a media release. “Isolated in 1942, streptothricin was the first antibiotic discovered with potent gram-negative activity. We find that not only is its activity potent, but it is highly effective against the most resilient contemporary multidrug-resistant pathogens and it inhibits protein synthesis through a unique mechanism.”
The findings are published in the journal PLOS Biology.
3 situations people can encounter harmful superbugs:
- Hospitals: Despite being a place people go to get healthy, studies show antibiotic-resistant superbugs often contaminate hospital rooms, beds, and floors. A new study finds that these deadly bacteria can even make its way into the ICU. Researchers say an ICU in Hangzhou, China was entirely contaminated with a virulent strain that infected one in three patients — creating a nightmare for healthcare professionals.
- Meat: One of the strains people are most familiar with is E. coli, and meat products are a common source of these infections. Recently, researchers in Spain say they discovered multidrug-resistant E. coli strains in 40 percent of chicken, turkey, beef, and pork products for sale in shops across the country.
- Pets: Dogs and cats may be passing antibiotic-resistant “superbugs” to their owners, a new study warns. Researchers discovered one pet in the United Kingdom and six from Portugal were carrying similar antibiotic-resistant bacteria as their owners. These could include E. coli and other strains linked to pneumonia.
Globally, drug-resistant infections kill an estimated 700,000 people a year. That figure could rise to 10 million by 2050 without an effective defense, according to estimates.
South West News Service writer Stephen Beech contributed to this report.


I want to walk again I’m in pain every time I get up now in using a walk any suggestions by