HAMILTON, Ontario — Diabetes, arthritis, and multiple sclerosis can all trace their origins back to the Black Death, according to new research. Researchers from McMaster University say the bubonic plague that ravaged Middle Age Europe fueled genes that make people vulnerable to autoimmune diseases today.
The Black Death shaped human evolution by influencing responses against pathogens, and pandemics could continue to do so in the future, warn scientists. Natural selection occurred at pace in survivors, leaving their descendants at increased risk, their research shows.
“When a pandemic of this nature – killing 30 to 50 percent of the population – occurs, there is bound to be selection for protective alleles in humans, which is to say people susceptible to the circulating pathogen will succumb. Even a slight advantage means the difference between surviving or passing. Of course, those survivors who are of breeding age will pass on their genes,” explains evolutionary geneticist Hendrik Poinar, director of McMaster’s Ancient DNA Center, in a university release.
How did the plague lead to the body attacking itself?
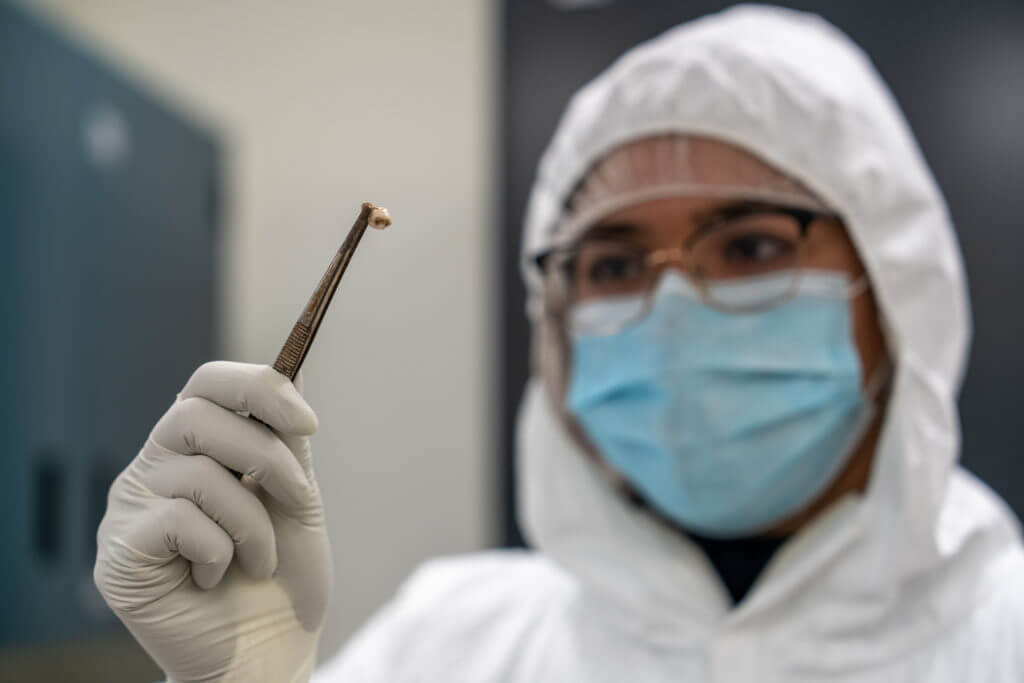
The findings are based on 516 ancient DNA samples extracted from the teeth of individuals who died before, during, or soon after outbreaks in the United Kingdom and Denmark. A century-long “window” enabled the international team to identify genetic differences that dictated who survived the virus.
Some were from the remains of corpses dumped in a mass grave in East Smithfield outside London. Historical records and radiocarbon dating revealed they all died between 1348 and 1349. Analysis showed those with a protective variant known as ERAP2 were around 40 to 50 percent more likely to survive.
“The selective advantage associated with the selected loci are among the strongest ever reported in humans showing how a single pathogen can have such a strong impact to the evolution of the immune system,” says human geneticist Luis Barreiro, a professor in Genetic Medicine at the University of Chicago.
Over time, our immune systems have evolved to respond in different ways to pathogens. It is a delicate balancing act. Some variants increase the risk of autoimmune diseases like rheumatoid arthritis and Crohn’s disease. It may not have mattered during the Black Death, as the urgency made the trade-off inevitable. So, what had once been a protective gene against plague in the Middle Ages leads to increased susceptibility to illness today.
Autoimmune diseases occur when the body’s natural defense system can’t tell the difference between your own healthy cells and foreign bodies. The body mistakenly attacks itself. There are more than 80 types that affect a wide range of organs.
The Black Death is the deadliest pandemic recorded in history
The bubonic plague claimed up to 200 million lives between 1346 and 1353. It was caused by the bacterium Yersinia pestis carried by fleas and spread across Europe, the Middle East, and northern Africa — killing up to half the population.
The findings suggest little to prior immunological adaptation to the bug. In subsequent bubonic plague outbreaks over the next 400 years, mortality rates decreased. This could have been the result of changing cultural practices, pathogen evolution, or human genetic resistance.
The researchers found evidence for positive selection of mutations in immune-related genes during and after the Black Death. They identified 245 variants that were “highly differentiated” when comparing pre and post-Black Death samples from London — four of which were replicated in the Danish sample group.
Individuals who carried some or all probably had immune defenses that responded efficiently to Y. pestis, and, as a result, had much better odds of surviving infections. Study authors add that the variants have a connection to protection from Y. pestis and overlap with mutations associated with increased susceptibility to autoimmune diseases.
The findings highlight the role past pandemics may have had in shaping present-day disease risk. The Black Death remains the single greatest human mortality event in recorded history, wiping out communities in some of the most densely populated areas.
Those with two identical copies of ERAP2 survived the pandemic at a much higher rate than peers with the opposing set. They neutralized Y. pestis by immune cells. Europeans living at the time were initially very vulnerable because they had had no recent exposure to Yersinia pestis. As waves of the pandemic occurred again and again over the following centuries, mortality rates decreased.
“Understanding the dynamics that have shaped the human immune system is key to understanding how past pandemics, like the plague, contribute to our susceptibility to disease in modern times,” says Poinar.
The study, published in the journal Nature, is the result of seven years of work that took an unprecedented look at the immune genes of victims of the Black Death.

South West News Service writer Mark Waghorn contributed to this report.

You refer to the Black Death as a virus several times in this article.
This is totally incorrect. Yersinia pestis was a bacterial infection.
Please fix this. The reference to this as a virus basically makes this article “unbelievable”.