CHICAGO — The brain cancer glioblastoma has one of the worst survival rates among patients. One of the reasons for this is strong chemotherapy treatments can’t reach tumors inside the brain. For the first time, however, Northwestern University researchers have successfully opened the blood-brain barrier to allow cancer drugs through to the brain using an implantable ultrasound device.
“This is potentially a huge advance for glioblastoma patients,” says lead investigator Dr. Adam Sonabend, an associate professor of neurological surgery at Northwestern University Feinberg School of Medicine and a Northwestern Medicine neurosurgeon.
The blood-brain barrier is a microscopic structure that protects the brain from harmful particles that may circulate through the body. This barrier, unfortunately, also often keeps out other substances that may help patients — like medication. This is why treating brain cancer is difficult. To treat the disease, intervention usually entails removal of the entire tumor (or as much as possible) since most drugs are off the table. This is why scientists continue to race against time for new, effective interventions that better serve glioblastoma patients.

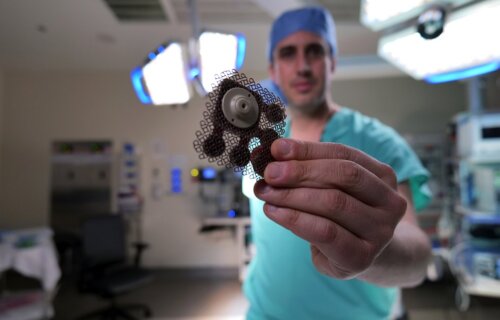
To conduct this study, researchers delivered a combination of paclitaxel and carboplatin, two strong chemotherapy drugs doctors don’t typically use in brain cancer treatments, to the brains of patients via the ultrasound implant every three weeks. The entire procedure is relatively simple, lasting four minutes, and allows patients to go home right after.
The team found that opening the blood-brain barrier resulted in around a four to six-fold increase in drug concentrations in the human brain. Further, the researchers were able to capture how fast the barrier closes after the ultrasound therapy, reporting that it happens in the first 30 to 60 minutes. This specific finding will help enhance drug delivery efforts and maximize how well the drug penetrates the brain.
“There is a critical time window after sonification when the brain is permeable to drugs circulating in the bloodstream,” explains Sonabend in a university release.
This work was a phase 1 human clinical trial, and the results have paved the way for the ongoing phase 2 trial that the scientists are conducting for patients with recurrent glioblastoma. The goal of this next trial is to see how the chemo combination might prolong the lifespan of these patients.
Scientists are hopeful that this work has the potential to improve outcomes not only for patients with aggressive brain cancers like glioblastoma, but other debilitating brain diseases as well.
“While we have focused on brain cancer (for which there are approximately 30,000 gliomas in the U.S.), this opens the door to investigate novel drug-based treatments for millions of patients who suffer from various brain diseases,” Sonabend concludes.
The findings are published in the journal The Lancet Oncology.