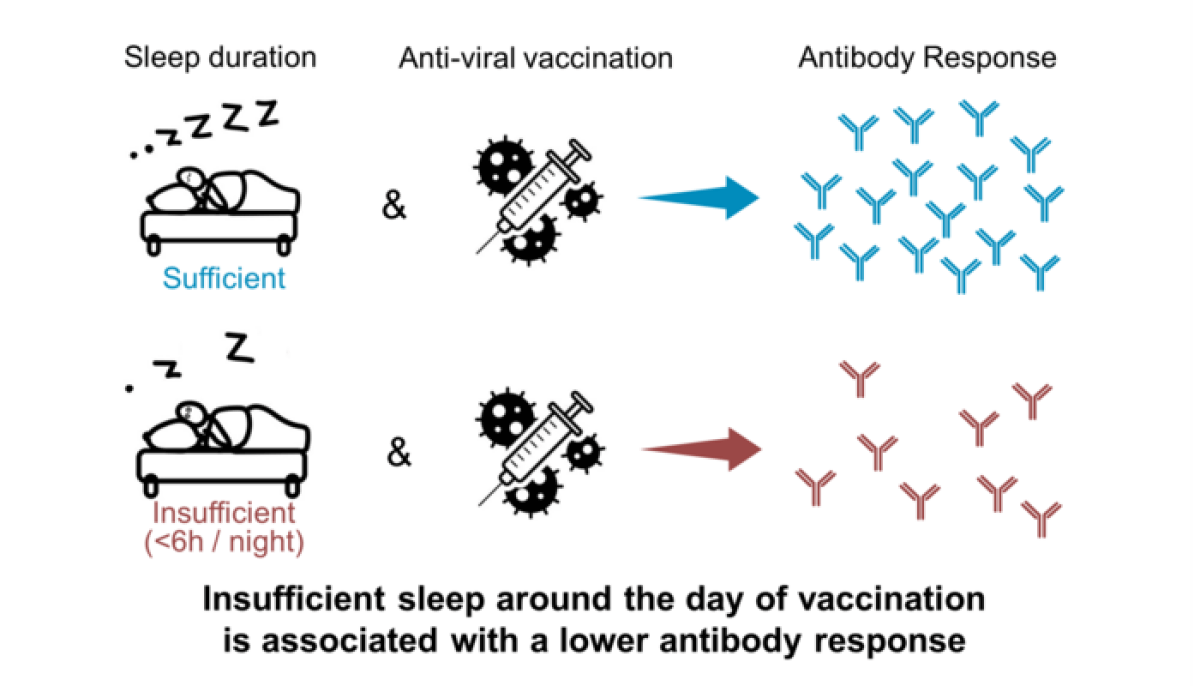
LOS ANGELES — A good night’s sleep boosts the power of vaccines, a new study suggests. Scientists hope the findings will offer people some control over their immunity. Their study reveals that getting less than six hours of sleep at night produces significantly fewer antibodies in comparison to people who clock over seven hours of rest.
The deficit in immune response is the equivalent of antibodies waning after two months, according to University of Chicago and French National Institute of Health researchers. Men consistently faced the consequences of poor sleep, but its impact in women varied. Researchers put this down to female sex hormones fluctuating.
“Good sleep not only amplifies but may also extend the duration of protection of the vaccine,” says senior author Eve Van Cauter, professor emeritus at the University of Chicago, in the media release.
“When you see the variability in protection provided by the COVID-19 vaccines—people who have pre-existing conditions are less protected, men are less protected than women, and obese people are less protected than people who don’t have obesity,” Van Cauter continues. “Those are all factors that an individual person has no control over, but you can modify your sleep.”
Poor sleep weakens the antibodies in adults between 18 and 60 more than it does for people over 65 years of age. This was not surprising to the team, since older adults generally sleep less anyway, meaning there is less of an impact on their immune health. Results also revealed the same pattern when the team measured sleep with motion-detecting wristwatches, in sleep labs, and by self-reported evaluations.

The effect was stronger in studies using objective measures of sleep. Scientists add this is likely because participants are “notoriously bad” at estimating the amount of shuteye they get.
For the study, the team re-analyzed and summarized seven investigations into viral infections influenza and hepatitis A and B. They compared the antibody response for those who slept a “normal” amount — between seven and nine hours — with “short sleepers” who managed under six hours.
The study, published in Current Biology, also examined the differences between people under and over age 65, and between genders.
“We know from immunology studies that sex hormones influence the immune system, says lead author Dr. Karine Spiegel, French National Institute of Health and Medicine.
“In women, immunity is influenced by the state of the menstrual cycle, the use of contraceptives, and by menopause and post-menopausal status, but unfortunately, none of the studies that we summarize had any data about sex hormone levels,” Dr. Spiegel concludes.
“We need to understand the sex differences, which days around the time of vaccination are most important, and exactly how much sleep is needed so that we can give guidance to people. We are going to be vaccinating millions and millions of people in the next few years, and this is an aspect that can help maximize protection.”
South West News Service writer Pol Allingham contributed to this report.

