KILDARE, Ireland — A popular drug doctors typically prescribe to treat obesity and Type 2 diabetes may hold cancer-killing benefits as well, according to new research. A team from Maynooth University explains that glucagon-like peptide (GLP-1) analogues are already a gold-standard pharmacological approach for fighting obesity, but these latest findings show that the treatment is also capable of reinvigorating the human body’s natural cancer-fighting mechanisms.
Estimates show that roughly one out of three U.S. adults is obese, while on a global scale, about 13 percent of the adult population is extremely overweight. Obesity-linked cancers, shockingly, make up 40 percent of all cancers doctors diagnose in the United States annually.
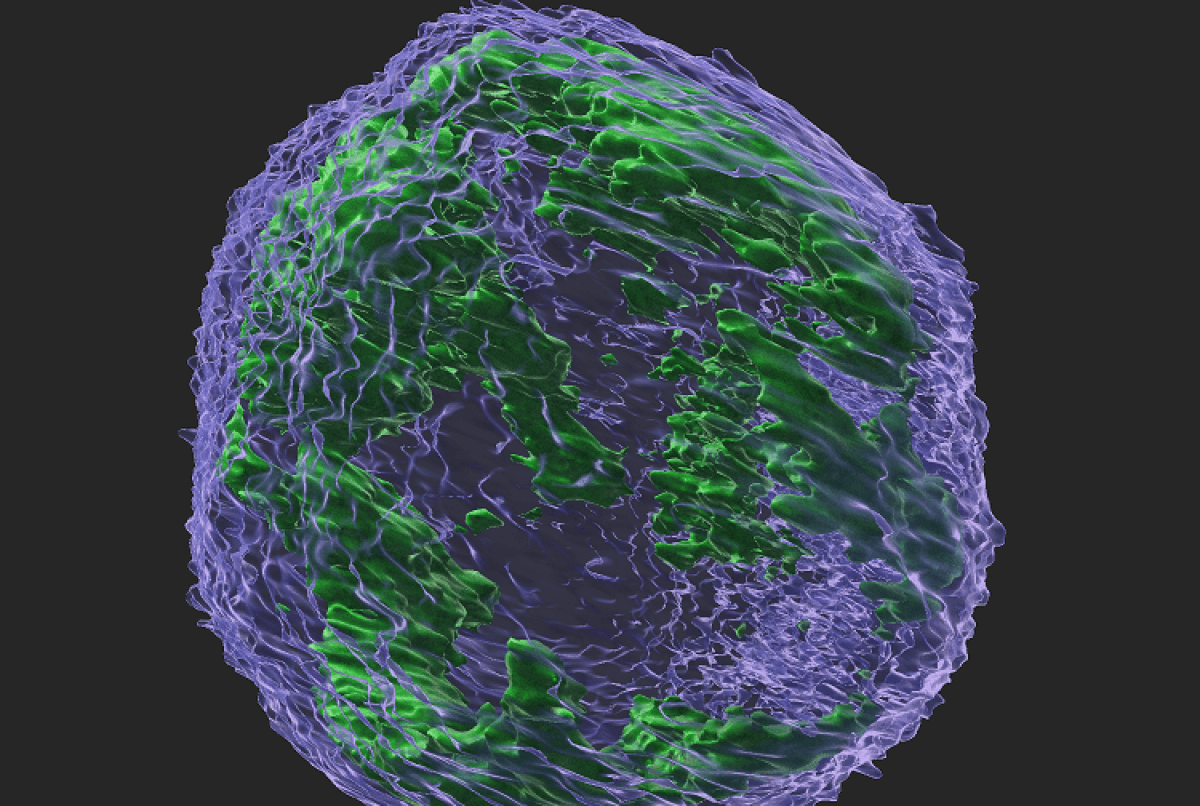
Studies continue to reveal that obesity and excess weight contribute to a long list of health concerns and risks, including cancer. Prior studies have found that people with obesity appear more likely to develop cancer, in part due to their anticancer immune cell (the ‘Natural Killer (NK)’ cell) being rendered useless, or neutralized, by obesity.
However, study authors report GLP-1 can restore the NK cell function in the body — including its ability to kill cancer cells. The project also notes that this restored cancer-killing effect on NK cells occurs independently from GLP-1’s main weight loss function. This suggests, researchers explain, that the treatment directly jumpstarts the NK cells’ engine.
Scroll down to see 3 varieties of GLP-1 drugs available
“My team and I are very excited by these new findings in relation to the effects of the GLP-1 treatment on people with obesity and it appears to result in real tangible benefits for those currently on the drug,” says Dr. Andrew E. Hogan, Associate Professor & Principal Investigator, Lonsdale Human Health Institute in Maynooth University, in a media release.
“While these findings will understandably be welcomed by those living with obesity and looking for safe and effective treatments, given the recent spike in popularity related to the benefits of the GLP-1 treatment with global and high-profile celebrities commenting on its success, global demand has increased and resulted in a worldwide shortage of the drug,” the researcher continues. “I hope this is something that is brought under control to ensure as many people as possible living with obesity can start their own treatment of this beneficial drug.”
“People with obesity can develop a variety of health problems like Type 2 diabetes, sleep apnea and cancer. These can have very negative impacts on their quality of life. This research and other promising findings on improvements in cardiovascular health after GLP-1 therapy indicate its potential benefits in addition to weight-loss,” explains Conor de Barra, PhD student in immunology at Maynooth University and Irish Research Council Scholar, who led the work in Dr. Hogan’s lab.
“We are finally reaching the point where medical treatments for the disease of obesity are being shown to prevent the complications of having obesity. The current findings represent very positive news for people living with obesity on GLP-1 therapy and suggest the benefits of this family of treatments may extend to a reduction in cancer risk,” concludes Prof. Donal O’Shea, HSE National Lead for Obesity & Principal Investigator.
What makes GLP-1 such a good weight loss drug?
GLP-1 receptor agonists have gained interest as potential obesity treatments due to their multifaceted effects on glucose metabolism, appetite regulation, and weight loss. These drugs mimic the action of the naturally occurring GLP-1 hormone and exert their effects by binding to and activating GLP-1 receptors in various tissues.
As obesity drugs, GLP-1 receptor agonists primarily work by either suppressing appetite, slowing gastric emptying, modulating glucose metabolism, or altering fat metabolism.
Several GLP-1 receptor agonists, such as liraglutide, semaglutide, and exenatide, have been approved for the treatment of Type 2 diabetes. Some of these drugs, specifically liraglutide and semaglutide, have also been approved for weight management in patients with obesity or overweight individuals with weight-related comorbidities.
The study is published in the journal Obesity.


Everyone with cancer should be able to try these drugs. My friend has glioblastoma which is fatal. He should be able to be treated with the hope of a cure. If the treatment causes a swifter death instead of a cure what would it matter? He is going to die without it, he may be cured with it.
Lisa, you are a great friend! What physicians are studying currently is the cancer-fungus link. Both of the diabetes drugs mentioned in this article have antifungal properties, so of course they may help your friend. Better, your friends Dr should know that in 2015, the toenail antifungal drug, Itraconazole (Sporanox) was approved for cancer treatment. Yes, glioblastomas seem to be helped with this drug. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4203550/. Additionally, given that fungi thrive on carbohydrates, if this glioblastoma is a fungal driven cancer, I’d be careful eating too many carbs. Hope this helps!