CHICAGO — Common painkillers can make the misery of osteoarthritis even worse, a new study warns.
Ibuprofen, naproxen, and diclofenac are among the many drugs for relieving aching joints. However, researchers say they may aggravate inflammation of the knee over time. They belong to a class of medications known as NSAIDS, or non-steroidal anti-inflammatory drugs. The study, based on a review of over 1,000 patients, is one of the first to investigate their long-term effects.
“To date, no curative therapy has been approved to cure or reduce the progression of knee osteoarthritis,” says lead study author Johanna Luitjens, M.D., a postdoctoral scholar in the Department of Radiology and Biomedical Imaging at the University of California-San Francisco, in a media release.
“NSAIDs are frequently used to treat pain, but it is still an open discussion of how NSAID use influences outcomes for osteoarthritis patients. In particular, the impact of NSAIDs on synovitis, or the inflammation of the membrane lining the joint, has never been analyzed using MRI-based structural biomarkers.”
Arthritis patients do better without the painkillers
The team found no benefit in 277 patients with moderate to severe osteoarthritis who also engaged in sustained NSAID use. In fact, joint inflammation and cartilage quality got worse over the next four years compared to a group of 793 controls who did not take the drugs.
Dr. Luitjens and her colleagues looked at the link between NSAIDs and synovitis and assessed how the therapy impacted joint structure over time.
“Synovitis mediates development and progression of osteoarthritis and may be a therapeutic target,” Dr. Luitjens continues. “Therefore, the goal of our study was to analyze whether NSAID treatment influences the development or progression of synovitis and to investigate whether cartilage imaging biomarkers, which reflect changes in osteoarthritis, are impacted by NSAID treatment.”
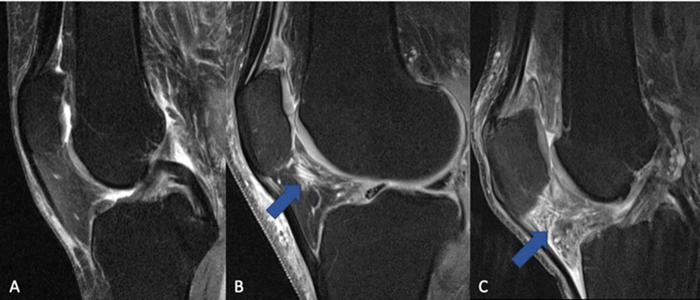
All participants underwent 3T MRI imaging of their knees at the start and end of the study period. This scan generates a magnetic field twice as strong as normal magnetic resonance imaging. Scans were scored for cartilage thickness, composition, and other measurements that served as non-invasive biomarkers of inflammation and arthritis progression.
“In this large group of participants, we were able to show that there were no protective mechanisms from NSAIDs in reducing inflammation or slowing down progression of osteoarthritis of the knee joint,” the study author reports. “The use of NSAIDs for their anti-inflammatory function has been frequently propagated in patients with osteoarthritis in recent years and should be revisited, since a positive impact on joint inflammation could not be demonstrated.”
1 in 4 deal with some form of arthritis
The CDC reports that about one in four U.S. adults (23.7%) or about 58.5 million people have a diagnosed case of arthritis. There are several possible reasons why NSAIDs increase synovitis.
“On the one hand, the anti-inflammatory effect that normally comes from NSAIDs may not effectively prevent synovitis, with progressive degenerative change resulting in worsening of synovitis over time,” Dr. Luitjens concludes. “On the other hand, patients who have synovitis and are taking pain-relieving medications may be physically more active due to pain relief, which could potentially lead to worsening of synovitis, although we adjusted for physical activity in our model.”
The study leader is calling for prospective, randomized studies to provide conclusive evidence of the anti-inflammatory impact of NSAIDs. Osteoarthritis is the most common form of arthritis, affecting more than 32 million adults in the U.S. and more than 500 million worldwide.
It occurs most frequently in the hands, hips, and knees. In patients, the cartilage that cushions the joint gradually wears away. Arthritis is often accompanied by inflammation, or swelling, of the joint, which can be extremely painful.
The study authors presented their findings at the annual meeting of the Radiological Society of North America (RSNA).
South West News Service writer Mark Waghorn contributed to this report.


I am a 67 year old female with severe osteoarthritis in my fingers especially on my dominant right side. It is a debiliating condition. I have been to many doctors and they have nothing to say except take Tylenol Arthritis. I would love to see some kind of hope for people like myself. After reading about this study it feels like there is no hope (or help) at all.
Well if you are taking Tylenol,, you may as well eat tic tax’s,, I live in severe pain, everyday of my life, all the discs in my back are collapsing, and there is nothing more they can do, I’ve already had 2 spine surgery’s and about 20 injections,, my pain Dr wants to cut my meds,, even tho I have referrals from my other drs, that tell him, my pain meds need to be upped,no pain meds,, that means no walking at all for me,, obviously,, my dr has never felt pain,, he can cut them,, if that makes him feel like a man,, I’ll always get them somewhere,, I’ll see him in court, so the ball is in his court, let me see, how he makes a move
This might help at least more food for thought
Dr John Bergman, DC. Yes, one of those healing modalities taught in US medical Schools until 1912 when Carnegie Rothschild & Rockefellers who had more money than God, took over, more $$$ from cheap coal tar poisons (most people) and continue to create the hype over us. Court ordered JAMA Med in 1963 to stop quacking the chiropractic profession. Been around longer
I was in a similar situation until I found a pain management specialist who listened. I now have a spinal cord stimulator implant that helped … but only somewhat. The game changer for me was a morphine pump implant. The morphine drips on to the spinal cord and is not processed thru the central nervous system, so no sleepiness, constipation or other side effects. It’s not a cure, but it changed my life. I can now function for 4 hours a day, sometimes more. Medtronics and Flowmax are the main manufacturers. IMHO Flowmax delivery system of the morphine is better. Hope this helps!
There is always hope !!!
Start you a list of seven things/people you are thankful for; then EVERY morning and throughout the entire day verbally tell what they are. WILL NOT take long until you can tell a difference in your pain !!!
I’ve tried everything to help my arthritis pain. None of the over the counter medications have ever helped. They can cause liver damage & vision loss. I’ve tried heat & ice therapies. The Drs even suggest doing exercises will help & made me go take Tai Chi classes. It doesn’t work. What a waste of time & effort.
I have Systemic Lupus as well and it took them 4 years to diagnose. 2 had 2 strokes, blood clots on my lungs and rashes and pain in my back and my knees is killing me. My joints is all tore up, I can barely walk. I have been to 2 pain clinics where they prod me with injections that only work for a day or two or not at all. I was taking Percocets on a regular and got afraid of addiction. So I took them only when I was I severe pain and the rest of the time I just dealt with the pain and my daily living just went down, I have gained so much weight. I can’t exercise it hurts too much. I no longer go to the pain clinic because if I don’t let them do the injection I can’t get my medication. So now at the young age of 64 I walk Bent over to compensate for the pain. I use creams and massage oils in the CBD family sometimes it helps and sometimes it don’t. I just don’t know what to do!! Just suffer? Day In and out I suffer in pain. I have a two story house I crawl up the stairs to get to my bedroom. I’m on a very limited income, I got a loaner scooter from the insurance company that sits in my house unused because I don’t have a ramp and nothing to carry it on if I go out, so I’m caught between a rock and a hard place. I just hope and pray for death and in the new world I will have a body that is in perfect condition that God has promised in his word the Bible.