CAMBRIDGE, Mass. — A robot pill that delivers insulin directly to the gut could replace multiple painful injections for people with diabetes. Researchers at the Massachusetts Institute of Technology say it can also deliver antibiotics, offering hope of battling superbugs with oral medications.
For patients and physicians, taking treatments orally is more desirable. Swallowing pills is safer, more convenient, and less invasive than other methods. However, some drugs often cannot withstand stomach acids before unleashing their payloads. The degradation makes them less effective.
The capsule, called RoboCap, could revolutionize modern medicine. In a swine model, it increased permeability for insulin by more than 10 times. Similar results were seen for pills containing vancomycin, an antibiotic that is usually delivered intravenously.
“Peptides and proteins are important drugs, but the degradative environment of the gastrointestinal tract and poor absorption has limited the ability to deliver these drugs orally,” says co-corresponding author C. Giovanni Traverso, MB, BChir, PhD, from the Division of Gastroenterology, Hepatology, and Endoscopy at the Brigham and the Department of Mechanical Engineering at MIT, in a media release.
Pigs have anatomical, physiological, and biochemical similarities to humans — making them ideal for research.
“RoboCap’s mucus-clearing and churning movements are designed to overcome these barriers and help deliver drugs to where they are needed,” Traverso adds.
How does RoboCap work?
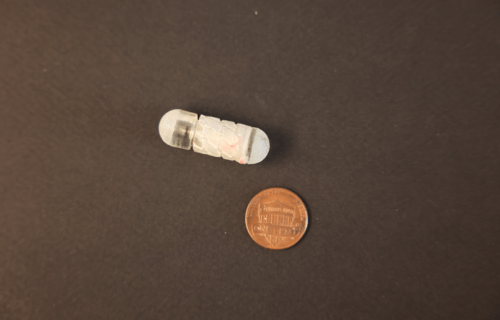
About the size of a blueberry, the inexpensive device is made from biodegradable polymer and stainless-steel components. It makes it through the harsh environment of the stomach, resisting attacks from enzymes, and penetrating the small intestine’s mucus barrier and other obstacles.
Currently, many common drugs including insulin must be delivered through other means. Study authors say when a patients ingests the new pill, RoboCap’s gelatinous coating dissolves in the stomach. The environment of the small intestine activates RoboCap, which vibrates and rotates to clear mucus. This enhances mixing and deposits the drug payload in the small intestine where the body absorbs the drug.
The team says their motivation was to make it easier for patients to take their medications, especially those needing frequent injections. The classic example is insulin, but there are many other medications people are currently unable to take in pill-form.
Diabetes is a global issue
Many diabetics require several doses of insulin to manage their condition daily. The standard delivery method is through injections with small needles many times a day. It can be especially uncomfortable, unwieldy, and is harder than just taking a pill. The Centers for Disease Control and Prevention reports that 37 million Americans – or more than one in 10 – suffer from diabetes.
It is the eighth-leading cause of death in America, responsible for just over 100,00 fatalities each year. Insulin is naturally produced in the pancreas, then travels to the liver where it helps process blood sugar. A person suffering from type 1 diabetes does not produce enough insulin to manage blood sugar. All patients require some sort of dosage to manage the condition.
Those with type 2 diabetes, the form linked to obesity, may also need insulin medication to boost levels of the hormone and manage their blood sugar. The standard injection of insulin is 100 international units (iu) per shot. A vast majority is lost during oral delivery.
Previous attempts to develop an insulin pill have had to carry around 500 iu to properly function.
Study authors describe RoboCap in the journal Science Robotics.
South West News Service writer Mark Waghorn contributed to this report.

Very nice modality of delivering insulin to intestine where the robocap vibrates and rotates to clear the mucus coating delivering the drug to the intestine from where it is absorbed in our system
Very nice system to deliver insulin because people generally get frustrated to get the needle pricking for managing their diabetes .