LOS ANGELES — Cedars-Sinai researchers say a new stem cell therapy procedure allows them to protect patients with ALS, or Lou Gehrig’s disease, and helps block muscle deterioration which normally occurs as a result of the fatal neurological disorder.
The Cedars-Sinai team successfully engineered and embedded protective proteins through the blood-brain barrier of patients with amyotrophic lateral sclerosis (ALS). The procedure increases hope that similar one-time treatments will greatly slow the disease’s degenerative effects, including limb paralysis and the loss of one’s ability to move, speak, or breathe. Researchers did not encounter any negative side-effects, while patients avoided leg paralysis following the transplant and replication of protein-producing stem cells from patients’ central nervous systems.
This breakthrough investigational therapy promotes the survival of motor neurons which typically degenerate in the spinal cord of patients with ALS. The researchers highlighted that none of the 18 people who underwent the stem cell gene therapy endured any serious side-effects after the transplantation.
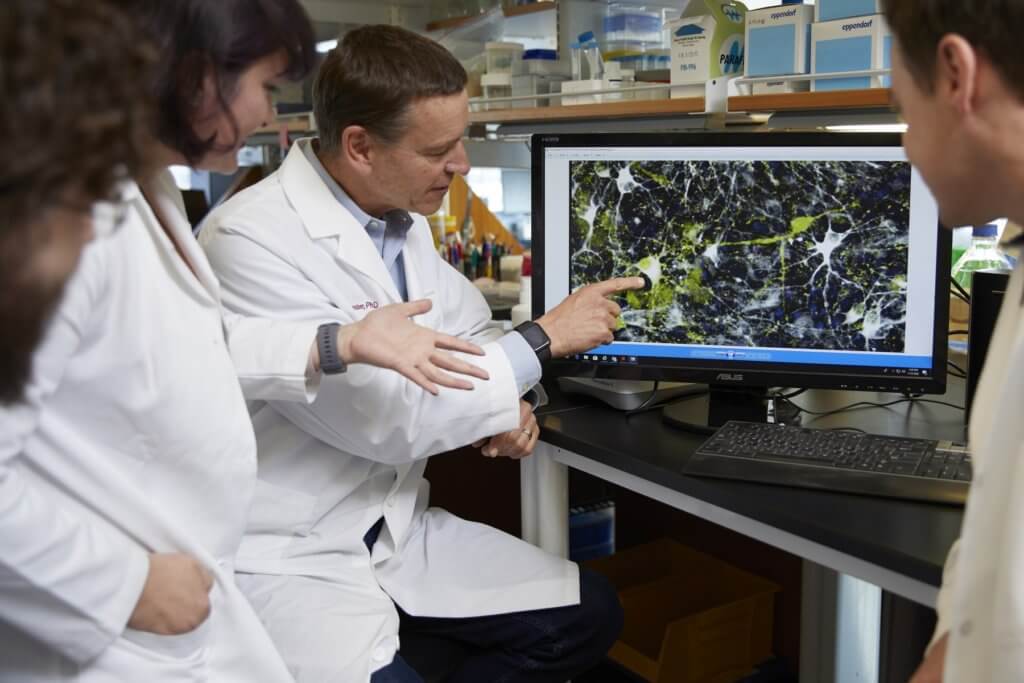
“Using stem cells is a powerful way to deliver important proteins to the brain or spinal cord that can’t otherwise get through the blood-brain barrier,” says corresponding author Clive Svendsen, PhD, professor of Biomedical Sciences and Medicine and executive director of the Cedars-Sinai Board of Governors Regenerative Medicine Institute, in a media release.
Just one treatment could last for 3 years
The safety of the trial and a lack of side-effects among patients is receiving praise from numerous scientists in the ALS and neurological research community.
“We were able to show that the engineered stem cell product can be safely transplanted in the human spinal cord. And after a one-time treatment, these cells can survive and produce an important protein for over three years that is known to protect motor neurons that die in ALS,” Svendsen says.
The researchers had several primary goals in this trial, which sought to show that stem cells engineered in Svendsen’s laboratory could produce the glial cell line-derived neurotrophic factor (GDNF), which help motor neurons pass signals between the brain and spinal cord. This process ultimately allows ALS patients to continue muscle movement which the disease typically destroys.
Prior to this recent study, neurological researchers feared there could be dire side effects or an inability to successfully bypass ALS patients’ blood-brain barrier using this therapeutic procedure. The blood-brain barrier, or BBB, serves as a structural and functional roadblock to potentially harmful microorganisms including parasites, viruses or bacteria in a person’s bloodstream.
“Because they are engineered to release GDNF, we get a ‘double whammy’ approach where both the new cells and the protein could help dying motor neurons survive better in this disease,” Svendsen added.
Researchers say they will soon build on the findings, published in the peer-reviewed journal Nature Medicine, including tests which target lower areas on the spinal cord and enrolling ALS patients in the study much earlier in their diagnosis.
“We are very grateful to all the participants in the study,” Svendsen concludes. “ALS is a very tough disease to treat and this research gives us hope we are getting closer to finding ways to slow down this disease.”

Did you ACTUALLY store the child’s cord blood cryogenically like my grandchildren’s have? Then you may not be successful.