OAK BROOK, Ill. – AI technology could lead to misinterpretations of mammograms, potentially putting patients at risk, according to a new study. Researchers contributing to the Radiological Society of North America warn that incorrect advice from AI-based decision support systems could seriously impair radiologists’ performance when reading mammograms — a key tool for detecting cancerous tumors.
Often heralded as a “second set of eyes” for radiologists, AI-based mammographic support systems show great promise. However, as technology advances, concerns arise that radiologists may come to favor AI suggestions over their own judgments when it comes to breast cancer.
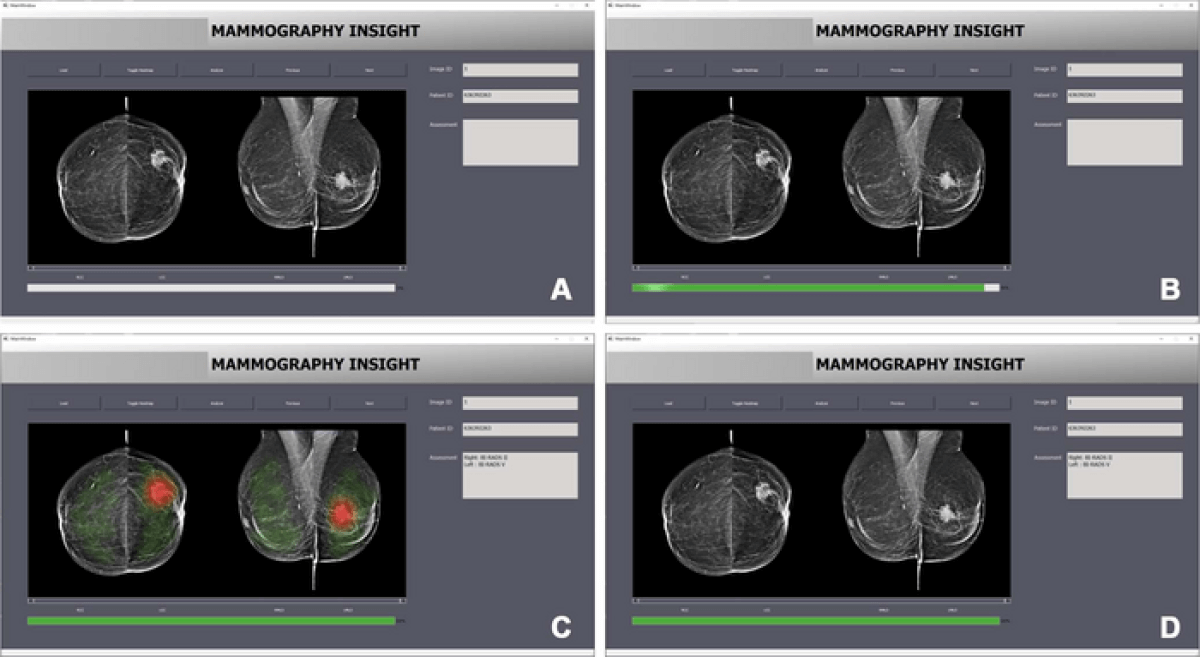
In the study, 27 radiologists read 50 mammograms and provided their Breast Imaging Reporting and Data System (BI-RADS) assessments with AI assistance. BI-RADS is a standardized system used by radiologists to describe and categorize breast imaging findings. While it does not provide diagnoses, it is crucial in helping doctors determine appropriate next steps in care.

Researchers presented the mammograms in two randomized sets. The first set of 10 included correct BI-RADS categories provided by the AI system. In the other set of 40 mammograms, the AI incorrectly assigned BI-RADS categories in 12 cases. The results revealed that radiologists were significantly worse at assigning correct BI-RADS scores when the AI suggested an incorrect category.
Inexperienced radiologists accurately assigned BI-RADS scores in nearly 80 percent of cases when the AI provided the correct category. However, when the AI suggested the wrong category, their accuracy dropped to less than 20 percent. Even experienced radiologists, with an average of over 15 years of experience, saw their accuracy decline from 82 percent to 45.5 percent when the AI suggested the wrong category.
“We anticipated that inaccurate AI predictions would influence the decisions made by radiologists in our study, particularly those with less experience,” says study lead author Thomas Dratsch, M.D., Ph.D., from the Institute of Diagnostic and Interventional Radiology at University Hospital Cologne in Germany. “Nonetheless, it was surprising to find that even highly experienced radiologists were adversely impacted by the AI system’s judgments, albeit to a lesser extent than their less seasoned counterparts.”
The researchers emphasize the importance of treating AI with care and considering the risks of using it.
“Given the repetitive and highly standardized nature of mammography screening, automation bias may become a concern when an AI system is integrated into the workflow,” Dr. Dratsch adds in a media release. “Our findings underscore the need for implementing appropriate safeguards when incorporating AI into the radiological process to mitigate the negative consequences of automation bias.”
The team suggests that radiologists should be shown the probability of each output and educate themselves about the reasoning process of the system. They should also feel accountable for their own decisions, as this could help reduce their bias towards relying on AI-generated results. The researchers plan to use tools like eye-tracking technology to better understand radiologists’ decision-making processes when using AI.
“Moreover, we would like to explore the most effective methods of presenting AI output to radiologists in a way that encourages critical engagement while avoiding the pitfalls of automation bias,” Dr. Dratsch concludes.
What is breast cancer?
Breast cancer is a type of cancer that originates in the breast tissue, typically in the cells that line the milk ducts (ductal carcinoma) or the lobules that produce milk (lobular carcinoma). It is the most common cancer among women worldwide, although men can also develop breast cancer, albeit at a much lower rate.
Cancer occurs when cells in the body grow uncontrollably, forming a mass or lump called a tumor. In the case of breast cancer, these abnormal cell growths can remain within the breast tissue or spread (metastasize) to other parts of the body, such as the lymph nodes, lungs, liver, or bones.
Risk factors for breast cancer include age, gender, family history, genetic mutations (e.g., BRCA1 and BRCA2), exposure to estrogen, personal history of breast conditions, obesity, alcohol consumption, and radiation exposure. However, it is important to note that having one or more risk factors does not necessarily mean a person will develop breast cancer.
Symptoms of breast cancer can vary but may include:
- A lump or thickening in the breast or underarm area
- Changes in breast size or shape
- Skin changes, such as dimpling, redness, or scaling
- Nipple discharge, inversion, or changes in appearance
- Pain or tenderness in the breast
Diagnosis of breast cancer typically involves a combination of physical examination, mammography, ultrasound, and biopsy. Treatment options depend on the stage and type of breast cancer, as well as the patient’s overall health and preferences. These options may include surgery, radiation therapy, chemotherapy, hormone therapy, targeted therapy, or a combination of treatments.
Early detection and advances in treatment have improved survival rates for breast cancer, highlighting the importance of regular screening and prompt attention to any potential symptoms.
The study is published in the journal Radiology.
South West News Service writer Alice Clifford contributed to this report.