SAN FRANCISCO — A common allergy drug may provide new hope for those dealing with the painful symptoms of multiple sclerosis (MS). Scientists at UC San Francisco have developed a method to measure the effectiveness of an over-the-counter antihistamine in repairing the brain, opening doors to evaluate future therapies for this debilitating disorder. The findings have significant implications for the development of treatments and offer hope to MS patients worldwide.
Led by physician-scientist Dr. Ari Green and neuroscientist Dr. Jonah Chan, the team utilized MRI scans to investigate the impact of clemastine, a common allergy medication previously identified as a potential MS therapy, on the brains of 50 participants enrolled in a clinical study.
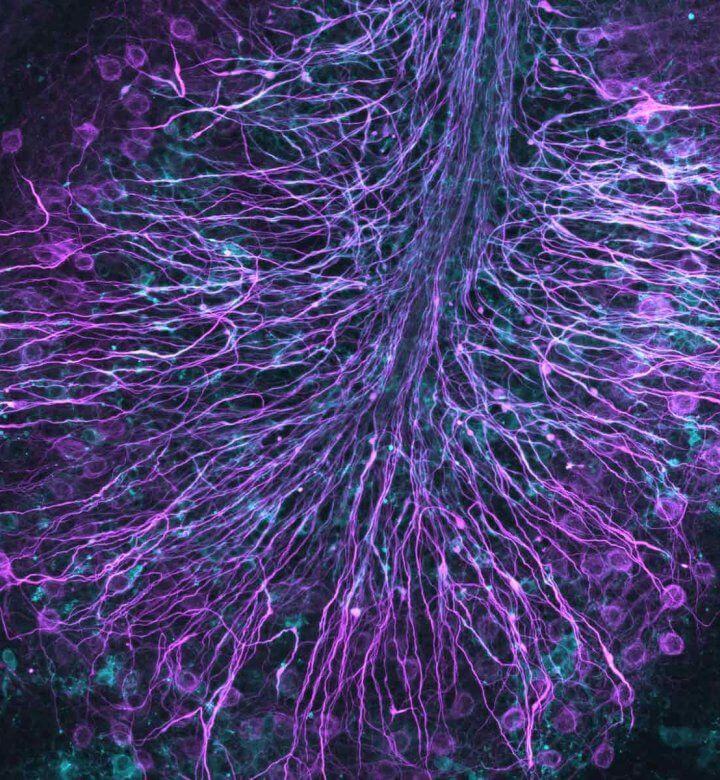
MS leads to the loss of myelin, the protective covering around nerve fibers. This loss results in delays in nerve signals and manifests in various symptoms such as chronic pain and fatigue, spasticity, vision loss, and cognitive impairment. By examining the myelin water fraction, a measure of myelin content derived from MRI imaging, the researchers were able to assess the effects of clemastine on myelin repair.
The study revealed that MS patients treated with clemastine experienced modest increases in myelin water, indicating successful myelin repair. The team also demonstrated that the myelin water fraction technique, when applied to specific regions of the brain, could effectively track the progress of myelin recovery.
“This is the first example of brain repair being documented on MRI for a chronic neurological condition. The study provides the first direct, biologically validated, imaging-based evidence of myelin repair induced by clemastine. This will set the standard for future research into remyelinating therapies,” says Dr. Green, the medical director of the UCSF Multiple Sclerosis and Neuroinflammation Center, in a university release.
Furthermore, the research revealed that myelin continued to increase even after clemastine treatment stopped. The study divided participants into two groups, with the first group receiving clemastine for the first three months and the second group receiving it from months three to five. Using the myelin water fraction as a biomarker, the researchers observed an increase in myelin water in the first group that persisted even after discontinuing the medication. Conversely, the second group experienced a decrease in myelin water during the placebo phase and a subsequent rebound after receiving clemastine.
The study’s findings align with previous research showing that clemastine can reduce delayed nerve signaling, potentially alleviating MS symptoms. The researchers focused on the corpus callosum, a brain region with high myelin content that connects the right and left hemispheres. Notably, significant myelin repair was observed outside the visible lesions commonly associated with MS, highlighting the need to target myelin restoration beyond these traditional lesion sites.
Unlike existing MS drugs that primarily modulate the immune system’s activity, clemastine works by stimulating the differentiation of myelin-producing stem cells. However, the medication has limitations, including sedation as a side-effect. The water fraction measurement technique emerges as a valuable tool in the development of more effective therapeutics for MS.
“Clemastine can only be partially effective at the doses we can use. We are hopeful that better medications will be developed, but clemastine has proven to be the tool to show remyelination is possible,” Dr. Green acknowledged.
Looking ahead, future research aims to explore clemastine’s potential in treating brain injury in premature infants, a population susceptible to myelin damage. Dr. Bridget Ostrem, a pediatric neurologist at UCSF Benioff Children’s Hospitals, is currently seeking FDA approval to initiate the first clinical trial evaluating clemastine for this debilitating condition.
The study is published in the journal PNAS.

Clemastine is a first generation antihistamine with serious side effects and not very effective in dealing with allergies. The study referred to did not deal with why it affects the myelin covering nor the potential dangers of increasing the water retention rates. Very irresponsible for that research to be released to the public since they may be prone to start self medicating. This is the danger of mixing research with profit motivations.