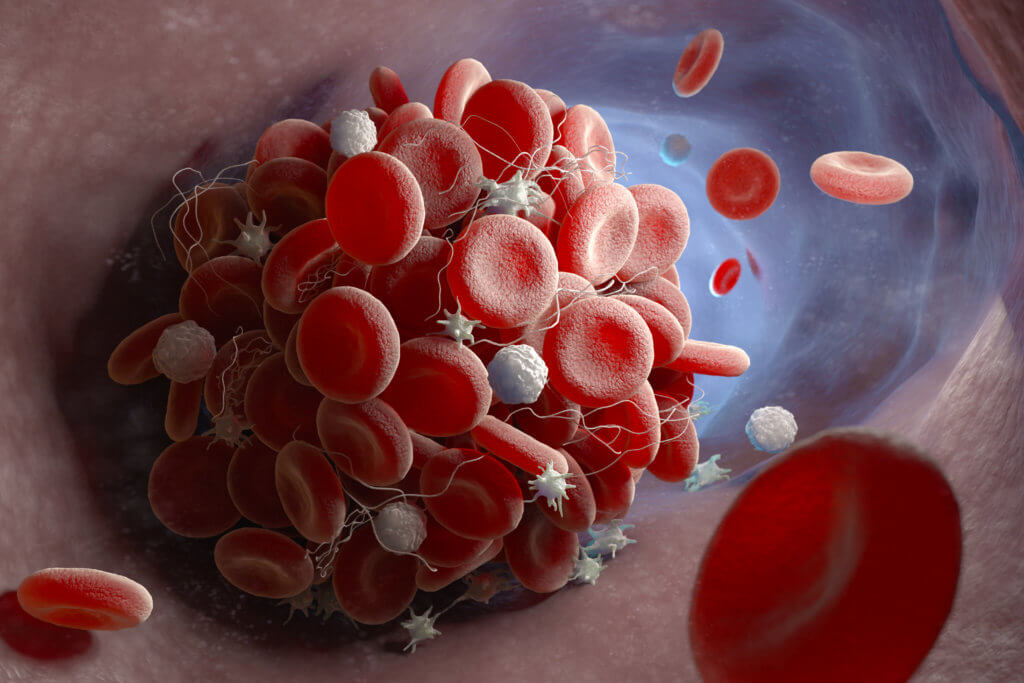
CHAPEL HILL, N.C. — A potentially deadly blood-clotting disorder has been linked to a common cold virus. For the first time, researchers from the University of North Carolina School of Medicine identified a connection between adenovirus infection, which typically results in cold and flu-like symptoms, and a rare blood clotting disorder — coupled with severe thrombocytopenia.
Platelets, often termed thrombocytes, play a crucial role in helping our blood clot when we have injuries. Sometimes, certain conditions can cause a drop in platelet levels, leading to a condition known as thrombocytopenia.
“This adenovirus-associated disorder is now one of four recognized anti-PF4 disorders,” says Dr. Stephen Moll, professor of medicine in the Department of Medicine’s Division of Hematology, in a university release. “We hope that our findings will lead to earlier diagnosis, appropriate and optimized treatment, and better outcomes in patients who develop this life-threatening disorder.”
The discovery provides new insights into the virus’ role in triggering what is known as an anti-platelet factor 4 disorder. This revelation opens new avenues of research to understand why and how this condition occurs.
Understanding the basics
Antibodies are proteins our body makes to fight off harmful invaders. However, in anti-PF4 disorders, the body mistakenly creates antibodies against a protein called platelet factor-4 (PF4), which is released by platelets. This results in excessive blood clotting and a drop in platelet levels.
There are various forms of this disorder. Sometimes, it is caused by exposure to a drug called heparin, leading to heparin-induced thrombocytopenia (HIT). In other cases, it appears without any known triggers, which is referred to as “spontaneous HIT.”
In recent years, a small number of cases of thrombocytopenia have been linked to specific COVID-19 vaccines, distinct from those produced by Moderna and Pfizer. This condition is termed vaccine-induced immune thrombotic thrombocytopenia (VITT).
Discovering the link
The pivotal moment came when a five-year-old boy, previously diagnosed with an adenovirus infection, was hospitalized with a severe blood clot in his brain and significantly reduced platelet levels.
“The intensive care unit physicians, the neuro-intensivist, and hematology group were working around the clock to determine next steps in the care for this young boy,” says Dr. Jacquelyn Baskin-Miller. “He wasn’t responding to therapy and was progressing quickly. We had questioned whether it could have been linked to his adenovirus considering the vaccine data, but there was nothing in the literature at that time to suggest it.”
The boy was found to have the antibody typically associated with HIT. A similar case was reported about another patient with an adenovirus infection, which led to more in-depth testing. These tests confirmed that the patients’ antibodies were targeting the same protein as HIT antibodies, concluding that they had a variant of HIT linked to the adenovirus infection.
What’s next?
This breakthrough leaves researchers with many unanswered questions, including how common this disorder is, if other viruses can cause it, and why not everyone with an adenovirus infection develops it.
“How common is the disorder?” asks Dr. Moll. “What degree of thrombocytopenia raises the threshold to test for anti-PF4 antibodies? And then finally, how do we best treat these patients to optimize the chance that they will survive such a potentially deadly disease?”
The study is published in the New England Journal of Medicine.
You might also be interested in:
- Common cold viruses can actually help defend against COVID-19
- Hibernating bears may hold the secret to preventing blood clots in humans
- Popular depression drug may also protect against heart disease, blood clots