LOS ANGELES — Scientists at UCLA have discovered a brain switch for obsessive-compulsive disorder, a new study reveals. It lies in an area known as the striatum, which is involved in decision-making and motor control. However, the team also finds that “helper cells” called astrocytes trigger these neurons, offering hope of new treatments for OCD.
“Our research has revealed a new cellular mechanism, which not only involves neurons – something we already knew – but also involves astrocytes, working together,” says corresponding author Baljit Khakh, a professor of physiology and neurobiology at the David Geffen School of Medicine at UCLA, in a university release. “Now we could expand our research in this area to cover additional mechanisms and cells.”
The breakthrough could lead to better therapies for a range of compulsive disorders. Uncontrollable urges can be life-threatening in certain circumstances. They can also lead to obesity, substance abuse, or financial ruin. Nearly one billion people worldwide suffer from obsessive-compulsive behaviors, yet our mechanistic understanding of them is still unclear, and effective therapeutics are largely unavailable.
They are highly prevalent in the general population and cause significant distress to the individual. Mental health charities report the number of people seeking help for obsessive-compulsive disorders has risen sharply since the beginning of the COVID-19 pandemic.
Recent research has found that COVID-19 can trigger and worsen obsessive-compulsive disorders. Stress and anxiety levels have increased among people, leading not only to psychological conditions, but also to increased risks of substance abuse.
READ: Don’t touch me: 2 in 3 people have become germaphobes since pandemic began
Experiments on mice discovered a protein associated with OCD and repetitive behaviors in neurons was also found in astrocytes. This suggests that therapeutic strategies targeting astrocytes and neurons may be useful for OCD and potentially other brain disorders.
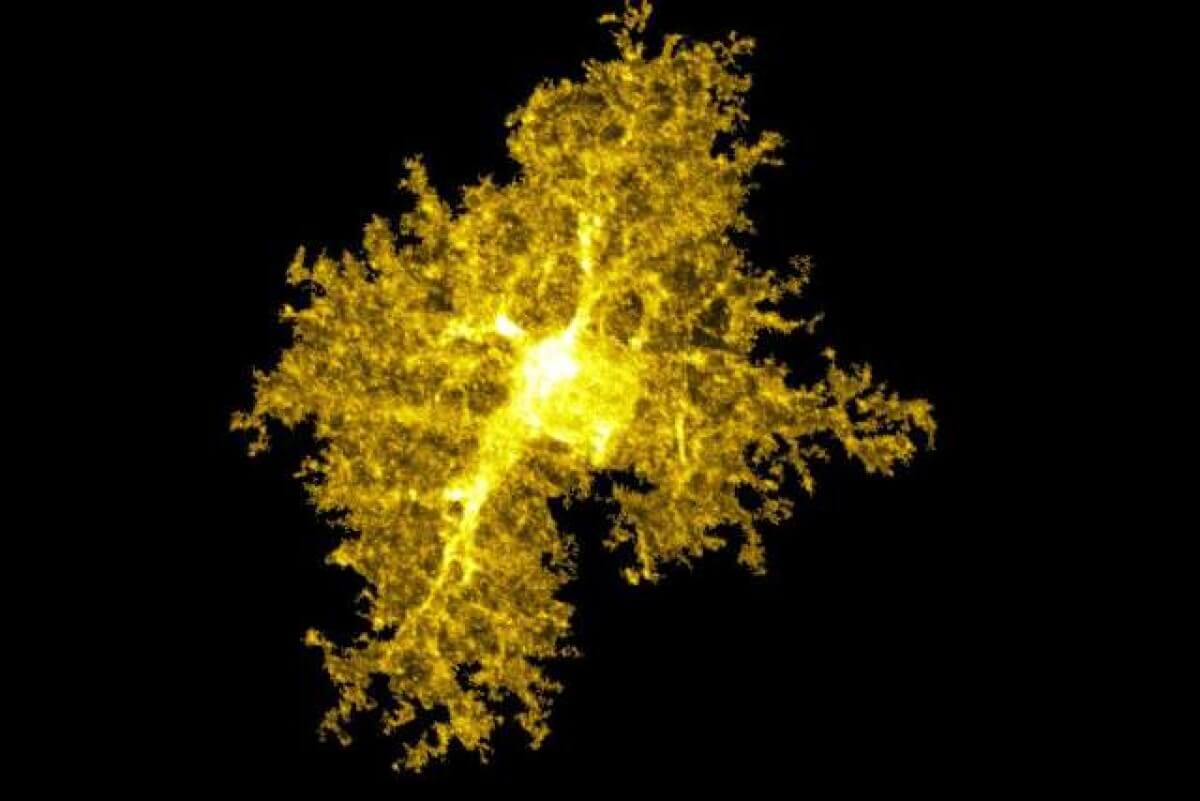
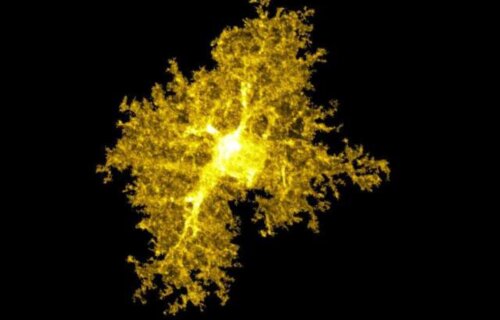
OCD, a lifelong anxiety disorder characterized by repetitive thoughts and actions, affects an estimated two to three percent of the U.S. population, though its prevalence may be higher due to underreporting and underdiagnosis. Psychotherapy, antidepressant medication, or both are typical treatments for OCD, but they can be ineffective for a sizable share of patients. Technological advances have made it more feasible to study astrocytes, which are complex cells.
“We really have to look at the proteins because they are very complex and diverse,” adds co-author Joselyn Soto, a neuroscience PhD student at UCLA’s medical school. “Depending on which cell expresses which proteins, we can predict the functions of that cell.”
The researchers used multiple approaches to isolate and visualize proteins across neurons and astrocytes within the striatum. When they compared proteins found in neurons and astrocytes, they unexpectedly discovered both contained a protein associated with OCD known as SAPAP3.
The researchers tested their findings by inserting the SAPAP3 protein back into neurons and astrocytes of mice that had been genetically modified to lack the gene that makes the protein. They found that the two types of cells interacted in different ways when they measured the protein’s effects on compulsion and anxiety, two of the typical hallmarks of OCD.
The mice no longer compulsively groomed themselves after the SAPAP3 protein was delivered back to astrocytes and neurons, suggesting that both types of cells could be valid targets for treatments aimed at curbing compulsion. However, only neurons with the SAPAP3 protein displayed an association with reduced anxiety in the mice, suggesting that astrocytes would not be a good target for anxiety treatments in OCD.
Soto notes that future research would delve deeper into how the interactions between these cells affect behavior.
“These are both major cell types – one doesn’t work without the other,” Soto says. “We really wanted to understand how these multicellular interactions within this brain region give rise to these complex behaviors, including compulsion and anxiety.”
The unexpected findings demonstrated the value of pursuing fundamental biology questions to help form new ideas about the basis of diseases.
“This started from a basic question: What proteins make up this complex cell?” Prof. Khakh concludes. “At the outset, we couldn’t have predicted its potential relevance to OCD.”
The study is published in the journal Nature.
South West News Service writer Mark Waghorn contributed to this report.