🔑 Key Findings:
- A new brain therapy clears harmful proteins linked to Alzheimer’s onset
- A gamma frequency of 40 Hz triggers the clearance of harmful brain waste
- The therapy focuses on light flickering and sound clicking to stimulate the brain
CAMBRIDGE, Mass. — Is a cure for Alzheimer’s disease finally on the horizon? In a revolutionary study, a team from The Picower Institute for Learning and Memory at the Massachusetts Institute of Technology (MIT) have unveiled a novel approach that could pave the way for new treatments for the deadly neurodegenerative disease. This method involves the use of light flickering and sound clicking at a specific frequency, which has been shown to promote the clearance of harmful proteins associated with Alzheimer’s through the brain’s specialized waste removal system.
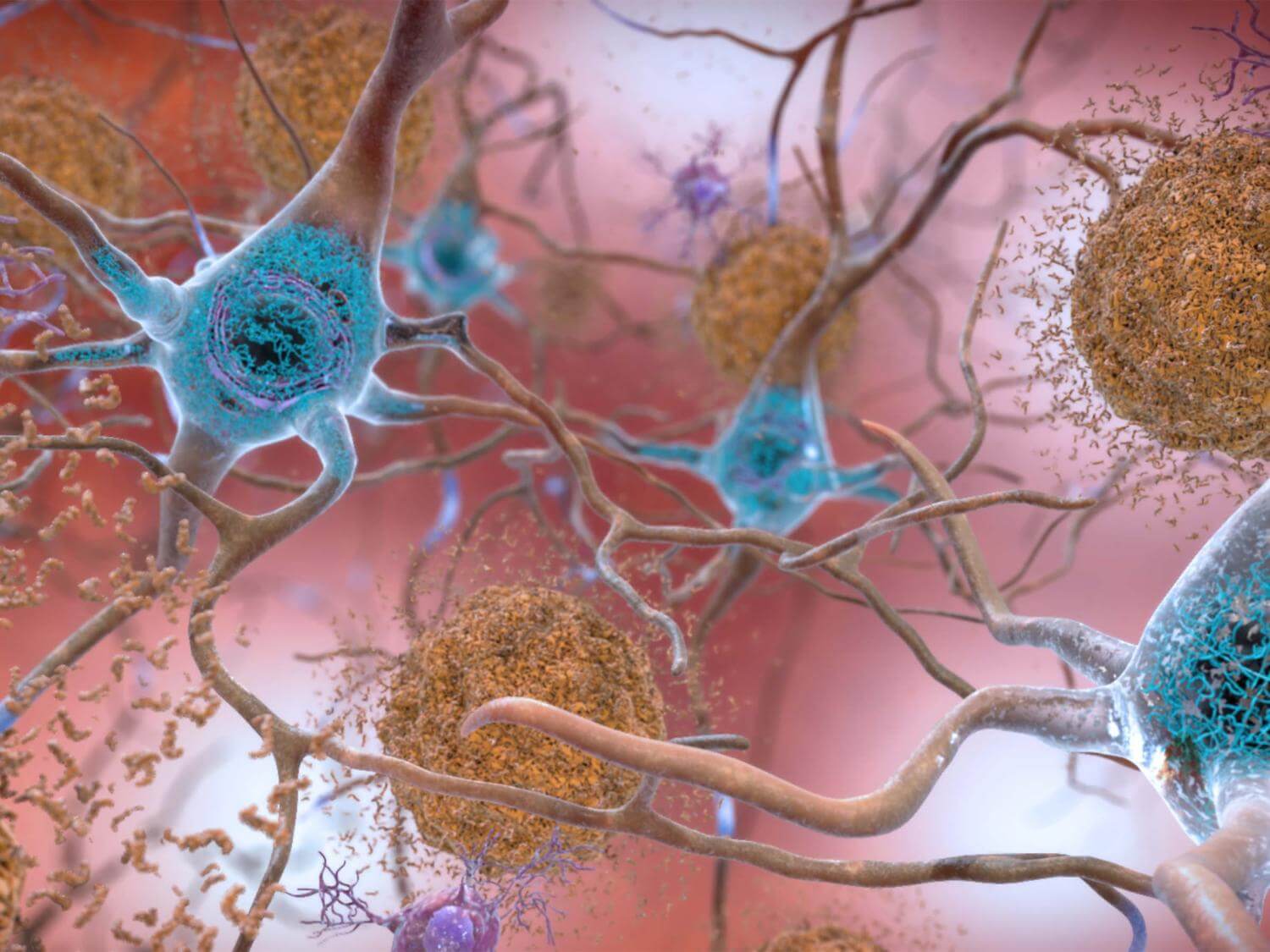
Alzheimer’s disease is characterized by the accumulation of amyloid proteins in the brain, which can lead to memory loss, cognitive decline, and ultimately, severe impairment. However, the new study suggests that stimulating the brain at a gamma frequency of 40 Hz can trigger a series of beneficial effects that help reduce these protein levels.
“Ever since we published our first results in 2016, people have asked me how does it work? Why 40 Hz? Why not some other frequency?” says study senior author Li-Huei Tsai, Picower Professor of Neuroscience and director of The Picower Institute and MIT’s Aging Brain Initiative, in a media release. “These are indeed very important questions we have worked very hard in the lab to address.”
Scientists embarked on a series of experiments using mice genetically modified to have Alzheimer’s disease. They discovered that this gamma frequency stimulation led to an increase in the release of certain peptides from a type of brain cell known as interneurons. These peptides, in turn, appear to play a crucial role in enhancing the brain’s glymphatic system, a recently discovered network that acts much like a plumbing system, clearing away waste products including amyloid proteins.
The glymphatic system operates alongside the brain’s blood vessels and is instrumental in the removal of brain waste. One key finding of the study is the role of the aquaporin 4 (AQP4) water channel found in astrocyte cells. These cells are vital for facilitating the exchange of glymphatic fluid. Researchers demonstrated that blocking the function of AQP4 with a chemical inhibitor or genetic disruption significantly reduced the beneficial effects of gamma frequency stimulation on amyloid clearance and cognitive function in mice.
“We do not yet have a linear map of the exact sequence of events that occurs,” notes Mitch Murdock, who led the experiments when he was a Brain and Cognitive Sciences doctoral student at MIT. “But the findings in our experiments support this clearance pathway through the major glymphatic routes.”
Another intriguing aspect of the study is the increase in vascular pulsatility observed in mice treated with gamma stimulation. This suggests that the stimulation not only affects the brain’s cellular activities but also has a broader impact on blood vessel function, further enhancing the glymphatic system’s ability to remove waste.
Using advanced RNA sequencing techniques, the team also identified changes in gene expression consistent with increased activity of AQP4 in astrocytes and an uptick in peptide production from interneurons. Notably, one peptide, VIP (Vasoactive Intestinal Peptide), known for its Alzheimer’s-fighting properties and role in regulating blood flow and glymphatic clearance, was found in higher levels in gamma-treated mice.
The implications of this study are significant, offering insights into how sensory stimulation of brain rhythms could potentially be harnessed to treat neurological disorders, including Alzheimer’s disease. While researchers caution that this mechanism is likely just one part of a complex puzzle, the findings represent an important step forward in understanding and combating this debilitating and incurable condition.
The study is published in the journal Nature.
You might also be interested in:
- Hope For Alzheimer’s Patients: Blocking One Protein May Stop Disease
- Nanoparticles may help untangle brain blockages caused by Alzheimer’s disease
- Drinking, vitamin D deficiency both linked to early-onset dementia
- Dementia did not exist in ancient Greece and Rome, study suggests
- Sitting all day linked to an early death — and exercise won’t help

I played this 40Hz sound https://www.youtube.com/watch?v=1_G60OdEzXs via my Sony MDR-7506 headphones: my jaw relaxed, after awhile my backbone was tingly, upper back muscles relaxed…