BARCELONA, Spain — “Living medicine” may help doctors tackle drug-resistant lung infections. A team in Spain says the breakthrough offers a new strategy to combat the leading cause of death in hospitals.
In experiments, the new treatment worked on mice infected with pneumonia. Antibiotic-resistant superbugs are one of the biggest threats facing mankind, according to the World Health Organization (WHO). The “living” medication uses a modified version of the bacterium Mycoplasma pneumoniae.
Scientists removed its ability to cause disease and repurposed the germ to attack drug-resistant infections instead. The modified bacterium works in combination with low doses of antibiotics that would otherwise not work on their own. The treatment doubled survival rates in the lab rodents. Additionally, a single, high dose showed no signs of toxicity.
Once the therapy finished its course, the innate immune system cleared the modified bacteria in a period of four days.
“We have developed a battering ram that lays siege to antibiotic-resistant bacteria. The treatment punches holes in their cell walls, providing crucial entry points for antibiotics to invade and clear infections at their source. We believe this is a promising new strategy to address the leading cause of mortality in hospitals,” says co-corresponding author Dr. María Lluch, Chief Scientific Officer at Pulmobiotics and a principal investigator at the International University of Catalonia, in a media release.
What makes certain lung infections so hard to treat?
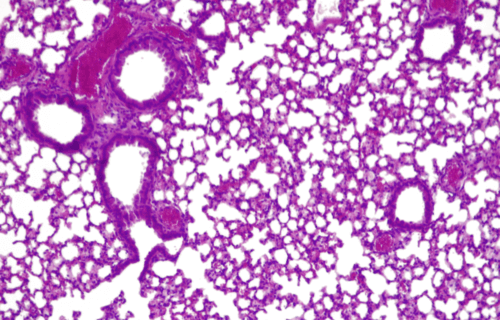
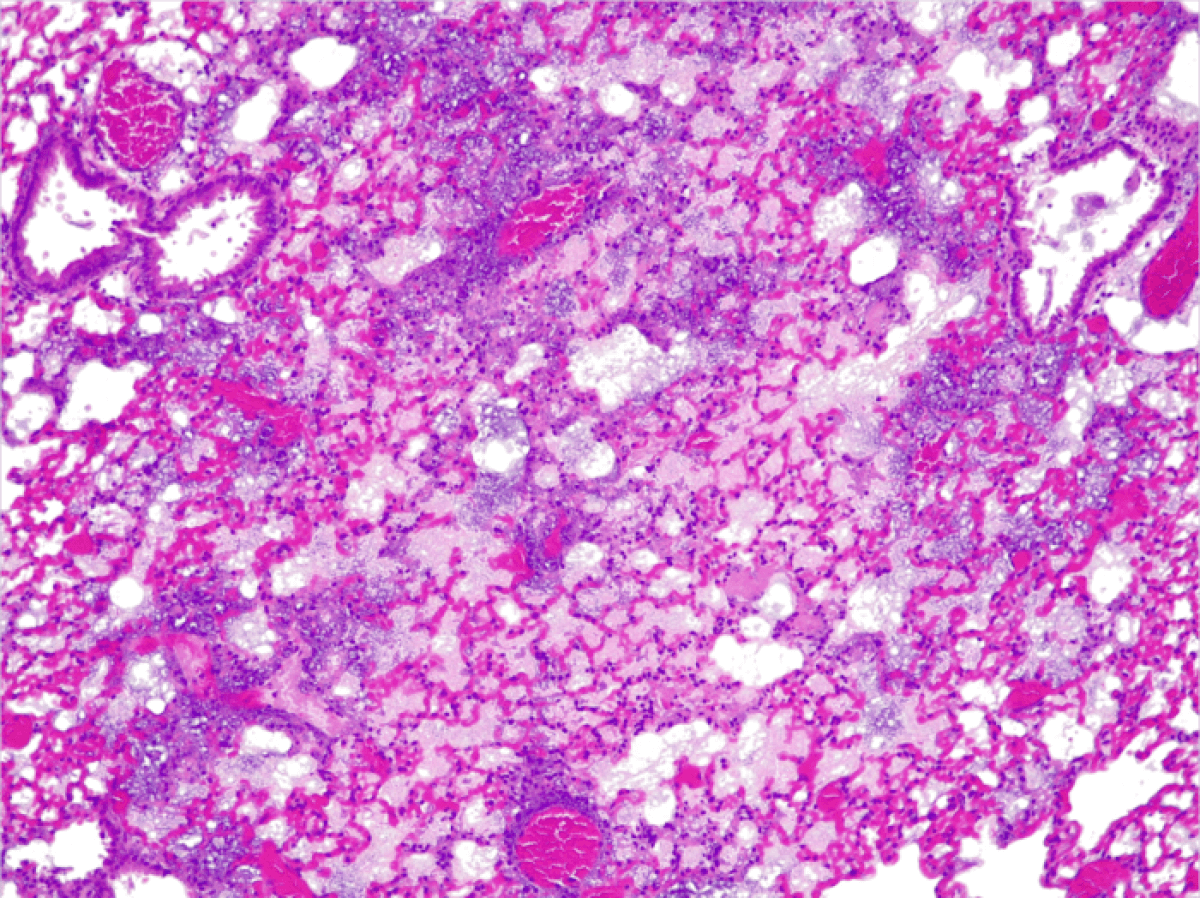
P. aeruginosa infections are difficult to treat because the bacteria lives in communities that form biofilms. They can attach themselves to various surfaces in the body, forming impenetrable structures that escape the reach of antibiotics.
Biofilms can also grow on the surface of endotracheal tubes used by critically-ill patients who require mechanical ventilators to breathe. This causes ventilator-associated pneumonia (VAP), a condition which affects one in four patients who require intubation. Infection incidence exceeds 50 percent for patients intubated because of severe COVID-19. VAP can extend a person’s time in the intensive care unit for up to 13 days and kills up to one in eight patients.
The Spanish team engineered M. pneumoniae to dissolve biofilms by equipping it with the ability to produce various molecules including pyocins. They are toxins naturally produced by bacteria to kill or inhibit the growth Pseudomonas bacterial strains.
To test its efficacy, researchers collected P. aeruginosa biofilms from the endotracheal tubes of patients in intensive care units. They found the treatment penetrated the barrier and successfully dissolved the biofilms. The researchers plan further tests before clinical trials begin.
How will patients receive this treatment?
Study authors expect that this treatment will be administered using a nebulizer, a device that turns liquid medicine into a mist which patients inhale through a mouthpiece or a mask. It opens the door to creating new strains of the bacteria to tackle other types of respiratory diseases such as lung cancer or asthma.
“The bacterium can be modified with a variety of different payloads – whether these are cytokines, nanobodies or defensins. The aim is to diversify the modified bacterium’s arsenal and unlock its full potential in treating a variety of complex diseases,” says ICREA Research Professor Dr. Luis Serrano.
The researchers are also using their expertise in synthetic biology to design new proteins that M. pneumoniae can deliver to patients. They are using these proteins to target inflammation resulting from P. aeruginosa infections.
Although inflammation is the body’s natural response to an infection, excessive or prolonged inflammation can damage lung tissue. The inflammatory response is orchestrated by the immune system, which releases mediator proteins such as cytokines. One type of cytokine (IL-10) has well-known anti-inflammatory properties and is of growing therapeutic interest.
“Live biotherapeutics such as M. pneumoniae provide ideal vehicles to help overcome the traditional limitations of cytokines and unlock their huge potential in treating a variety of human diseases. Engineering cytokines as therapeutic molecules was critical to tackle inflammation. Other lung diseases such as asthma or pulmonary fibrosis could also stand to benefit from this approach,” concludes Dr. Ariadna Montero Blay, co-corresponding author of the study in Molecular Systems Biology.
The study is published in the journal Nature Biotechnology.
South West News Service writer Mark Waghorn contributed to this report.