SEOUL, South Korea — Artificial intelligence (AI) may outperform humans in screening for lung cancer, one of the deadliest forms of the disease. A high-performance machine learning tool demonstrated increased sensitivity, meaning it was much less likely to overlook cases requiring immediate intervention.
The tool also improved radiologists’ performance in detecting tumors on chest X-rays and fostered greater human acceptance of AI technology. Recent studies have shed light on how helpful artificial intelligence can be for doctors when it comes to medical diagnoses.
“It is possible that the relatively large sample size in this study bolstered readers’ confidence in the AI’s suggestions,” says Dr. Chang Min Park from Seoul National University, the study’s lead author, in a media release. “We think this issue of human trust in AI is what we observed in the susceptibility in this study: humans are more susceptible to AI when using high diagnostic performance AI.”
The study showed that the successful identification of cancerous lung nodules on chest X-rays rose notably to 94% when computer data was employed. These abnormal growths typically develop following infections but, in rare instances, they can be indicative of cancer.
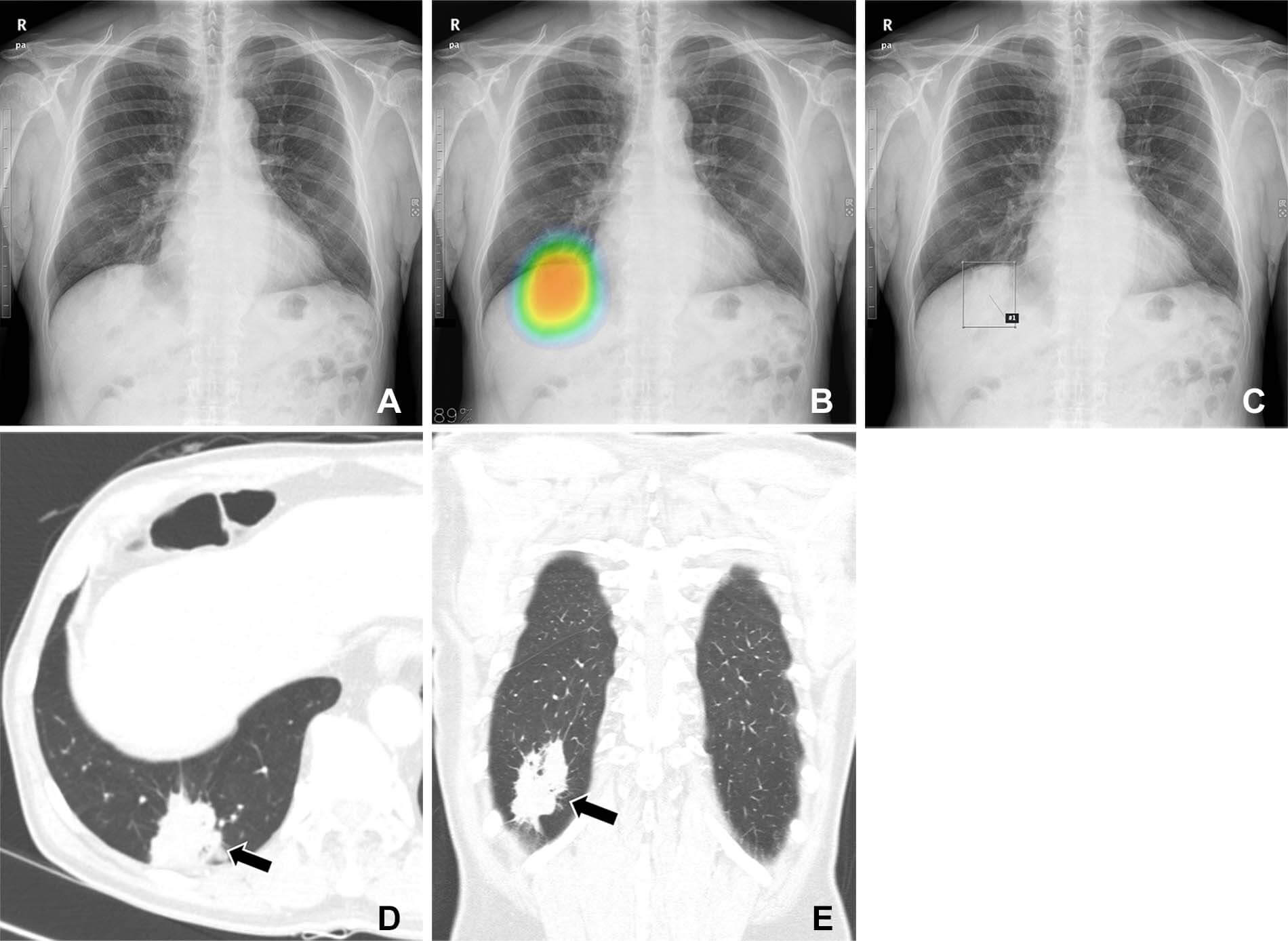
In the study, 20 thoracic radiologists with up to 18 years of experience and 10 students analyzed 120 chest X-rays without AI assistance. Half of these X-rays were from male lung cancer patients in South Korea, and the remaining half served as controls. In a follow-up session, each group re-evaluated the X-rays, this time aided by either high- or low-accuracy AI. Unbeknownst to the readers, two distinct AIs were used.
The study’s findings underscore the significance of employing “high diagnostic performance AI.” However, the researchers note that definitions can vary based on the task at hand and the specific clinical context.
While an AI model that can identify every abnormality might appear flawless, its practicality in reducing the workload in a mass screening scenario would be limited. “Therefore, our study suggests that clinically appropriate use of AI requires both the development of high-performance AI models for given tasks and considerations about the relevant clinical setting to which that AI will be applied,” says Dr. Park.
The researchers plan to extend their work on human-AI collaboration to other abnormalities detected on chest X-rays and CT images. Lung cancer is often diagnosed too late due to the lack of initial symptoms. Previous studies have demonstrated AI’s ability to predict colon diseases, Alzheimer’s, heart attacks, and dementia.
The study is published in the journal Radiology.
South West News Service writer Mark Waghorn contributed to this report.