BALTIMORE — Inflammation in the brains of children might be a cause for such autism and schizophrenia, according to a new study. The findings could pave the way for novel treatments of these significant neurological disorders in children.
The research, conducted by a team at the University of Maryland School of Medicine (UMSOM), shows that inflammation hinders certain neurons from maturing in a developing brain.
Clinically, severe inflammation early in life is already recognized as a risk factor for the onset of autism and schizophrenia. This study, for the first time, connects inflammation to the abnormal development of certain brain cells possibly linked to these neurodevelopmental disorders.
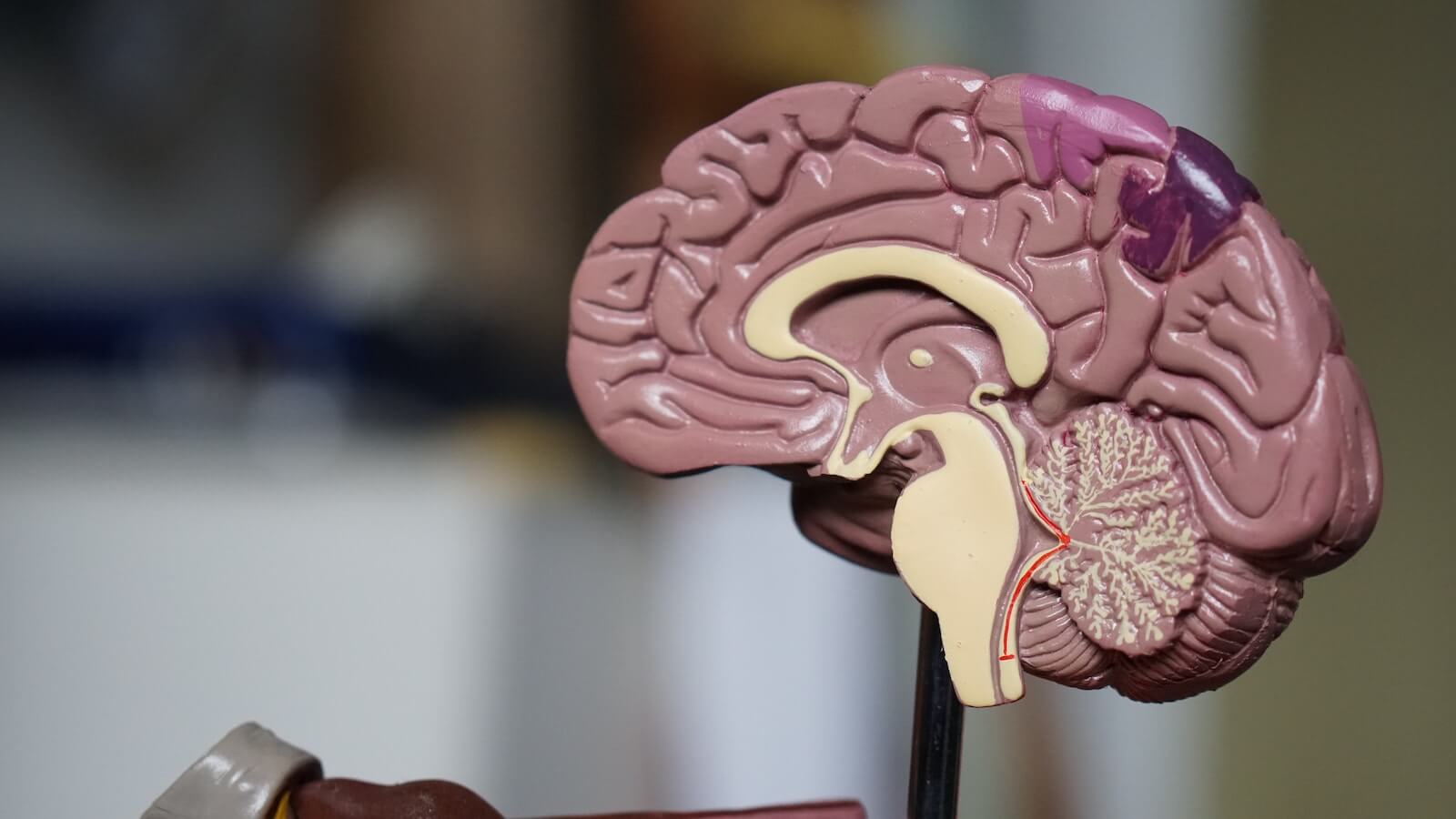
By utilizing single-cell genomics, the researchers examined the brains of children who succumbed to inflammatory conditions such as bacterial or viral infections or asthma, in comparison to those who died suddenly due to accidents. Their findings revealed that early childhood inflammation impedes the complete maturation of specific neurons in the cerebellum, a part of the brain essential for motor control and cognitive functions, including language, social skills, and emotional regulation.
Historically, infants with cerebellum abnormalities often exhibited signs of neurodevelopmental disorders. Similarly, animal models exposed to inflammation before birth have been observed to develop these disorders.
“We looked at the cerebellum because it is one of the first brain regions to begin developing and one of the last to reach its maturity, but it remains understudied,” says study co-leader Dr. Seth Ament, an associate professor in the Department of Psychiatry at UMSOM, in a media release. “With the fairly new technology of single nucleus RNA sequencing, we could look at the cell level to see changes in the brains.”
The study analyzed the post-mortem brain tissues of 17 children between the ages of one and five: eight from inflammatory conditions and nine from accidents. Notably, none had been diagnosed with a neurological disorder. The tissues had been amassed over many years by UMSOM.
“This has never been done before in this age group and in the context of inflammation,” adds study co-author Professor Margaret McCarthy. “The gene expression in the cerebella of children with inflammation were remarkably consistent.”
Two rare types of cerebellar neurons, Golgi and Purkinje, emerged as most susceptible to brain inflammation. On a cellular level, these neurons exhibited signs of premature developmental disruption.
“During development, Purkinje neurons form synapses connecting the cerebellum to other brain regions involved in cognition or emotional control, while Golgi neurons coordinate communication between cells within the cerebellum,” Dr. Ament explains. “Disruption of either of these developmental processes could explain how inflammation contributes to conditions like autism spectrum disorders and schizophrenia.”
Highlighting the intricate interplay between genetics, environmental factors, and inflammation, Dr. Ament stressed the need to comprehend specific cell roles in the brain and their genetic interactions to unearth treatments for various brain disorders.
“This study is one of the first to show that gene expression changes during inflammation may set the stage for later cellular dysfunction, such as reducing synaptic connectivity or altering energy metabolism. It’s critical to understand these mechanisms and changes at the cellular level during brain development in the hope that someday we can develop treatments for neurodevelopmental disorders,” says Professor Mark Gladwin, Dean of UMSOM.
This study is published in the journal Science Translational Medicine.
You might also be interested in:
- 1 In 4 Teens May Have An Undiagnosed Case Of Autism, Study Reveals
- Special blood factor linked to clotting can reverse brain aging
- Disturbing link discovered between popular weed killers and child brain dysfunction
South West News Service writer Stephen Beech contributed to this report.

