DARLINGHURST, Australia — A groundbreaking discovery by stem cell researchers could herald a new age of personalized medicine. Scientists in Australia have crafted an innovative technique that facilitates large-scale studies on the intricate relationship between human genetics and biology.
Stem cells possess the incredible ability to morph into various tissues, sparking hope for treating conditions such as spinal cord injuries, diabetes, Parkinson’s, Alzheimer’s, cardiovascular disease, and cancer. The recent breakthrough, as outlined in the journal Nature Communications, is projected to revolutionize therapies, making them more affordable, efficient, and safe.
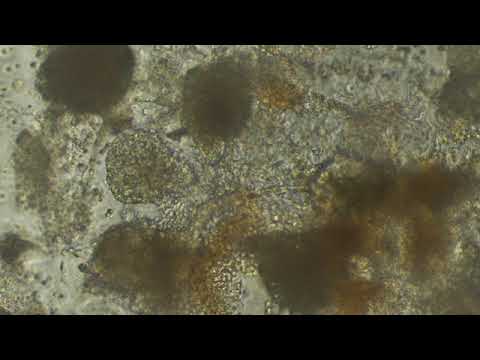
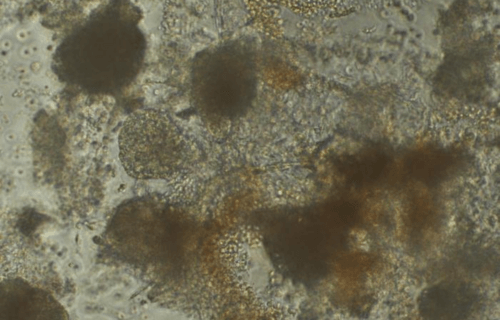
The Australian team has introduced an avant-garde “village in a dish” concept that allows the simultaneous growth and analysis of stem cells from a multitude of donors. This advancement amplifies the quality of studies 100 times.
“Our village model provides a powerful way to understand how genetic differences between people influence health and disease,” says Professor Joseph Powell, Director of Cellular Science at the Garvan Institute, and Director of the UNSW Cellular Genomics Futures Institute, in a media release. “Even though we share the majority of our DNA, variations in our genes lead to unique traits and responses. The village system captures this diversity at a large scale, revealing how genetic differences between people affect the complex mechanisms underlying biology and disease.”
How is this stem cell process different from controversial ones?
While the cells in the human body have preassigned roles, like nerve cells, liver cells, or muscle cells, stem cells bear the potential to mature into any cell type. As a result, they have emerged as a pivotal focus of medical research due to their regenerative capabilities.
Traditionally, the use of embryonic stem cells has incited ethical debates. However, Nobel Prize-winning research revealed that skin cells can be “genetically reprogrammed” to become stem cells, known as induced pluripotent stem cells (iPSCs).
Current methods depend on a technique known as “bulk RNA sequencing,” which averages the gene expression across different cell types into a single measure. This strategy tends to obscure potential variations among individual cells or cell types, yielding a partial or biased depiction of gene expression in the sample. Consequently, this could lead to erroneous or misleading conclusions.
Prof. Powell and his colleague devised a method that involves culturing stem cells from numerous donors in one dish and then subjecting them to single-cell sequencing. This approach safeguards the unique characteristics of individual cells, enabling precise snapshots of the entire population.
The village-in-a-dish technique enables expansive studies on human organ systems typically out of reach. By generating organ-specific cells from multiple individuals, the necessity for obtaining live tissue samples from donors is negated, overcoming the limitations of studying only a select few individuals’ cells.
For instance, this technique can offer insights into cardiac conditions by generating heart cells from thousands of individuals, a task unachievable through direct tissue sampling.
“Medical research often relies on animal models, which are not perfect physiological proxies for humans. Induced pluripotent stem cells, which can be generated from a patient blood sample, provide the complete DNA profile of the patient and then can be differentiated into almost any cell type in the human body,” Prof. Powell adds.
From a scientific standpoint, the stem cell-based system offers a powerful means of understanding the intricate relationship between human genetics and biology, which cannot be achieved through animal models. This breakthrough opens the door to expedited clinical trials that can predict how groups of patients may respond to drugs, leading to the discovery of new treatments.
“By studying cells from many individuals at once, we can identify genetic factors that influence disease and treatment response at an unprecedented scale,” says Dr. Drew Neavin, first author of the paper and postdoctoral scientist at Garvan.
“An example is assessing cardiac toxicity, or Lewy body accumulation in Parkinson’s disease across hundreds of cell lines derived from patients. Rather than reflecting single individuals, such studies would reveal shared and distinct responses among genetic groups. The insights could then inform clinical trials by pre-selecting patient populations likely to benefit. Overall, this approach could transform our ability to translate stem cell science into precision treatments,” the researcher concludes.
South West News Service writer Mark Waghorn contributed to this report.

Well, someday this is bound to be true, but up until now it’s either hidden away and saved for very rich people, or it’s just not there yet. DNA and cell biochemistry is probably the toughest problem in the universe, except for the mysteries of the human brain and intelligence.
We are very complex beings.