SAN DIEGO — A critical study is revealing the reason why vaccines for Staphylococcus aureus (SA) have consistently failed in clinical trials. Researchers from the University of California San Diego School of Medicine say that SA can manipulate the human immune system, leading to the ineffectiveness of vaccines.
Staphylococcus aureus, present in about 30 percent of the population, typically resides harmlessly in the nose. However, it is also a significant cause of infections acquired in hospitals and in public. Doctors have been searching for a vaccine against SA for a long time, but it has remained elusive.
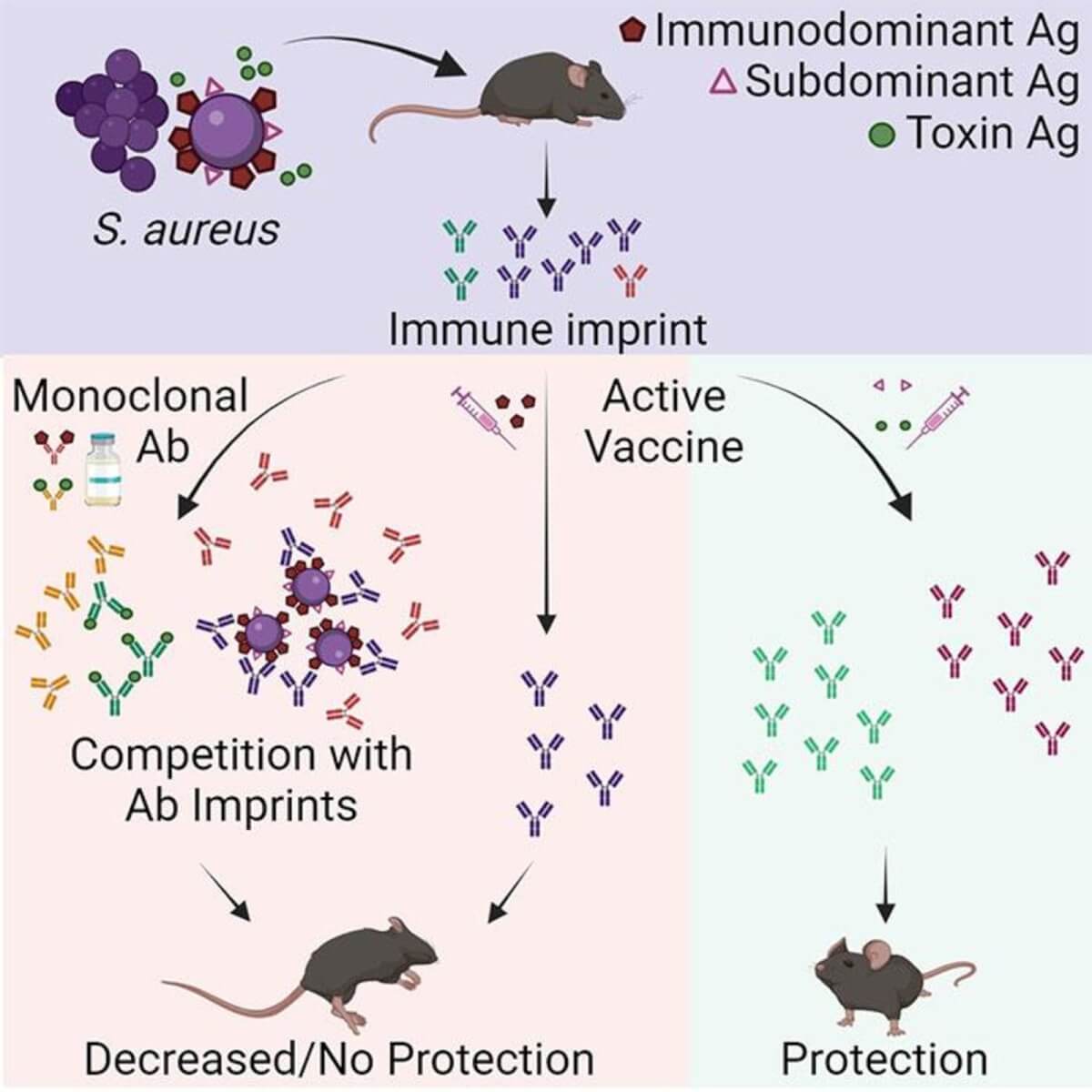
Researchers tested a new hypothesis. They suggested that SA bacteria initially trigger the release of non-protective antibodies in humans. When vaccinated, these ineffective antibodies are recalled, rendering the vaccine futile.
“SA has been with humans a long time, so it’s learned how to be part-time symbiont, part-time deadly pathogen,” says study senior author Dr. George Liu, professor in the Department of Pediatrics at UC San Diego School of Medicine, in a university release. “If we’re going to develop effective vaccines against SA, we need to understand and overcome the strategies it uses to maintain this lifestyle.”
The immune system typically produces protective antibodies against foreign molecules, known as antigens, and remembers them for future encounters. However, this only works if the initial response was protective, which is not the case with SA.
“What sets SA apart is that the bacteria themselves have ways of evading the immune system from the moment they encounter us, and these evasive strategies are only reinforced by vaccination,” notes study co-lead author Dr. JR Caldera, who completed his doctoral research in the Liu Lab.
The researchers’ approach involved analyzing blood serum from healthy volunteers for anti-SA antibodies, then transferring these antibodies to mice to test their protective capability and their influence on the efficacy of existing SA vaccine candidates. Their findings showed that the vaccines failed in mice with human anti-SA antibodies or previous SA exposure. However, in mice without such exposure, the vaccines were effective. This discrepancy aligns with the failure of SA vaccines in human trials, unlike previous mouse studies.
Interestingly, the team discovered that the type of antibodies matters. Antibodies targeting SA’s cell walls, which most current vaccines are based on, were ineffective. In contrast, antibodies aimed at the toxins produced by SA successfully neutralized them.
“One pathogen can have many different antigens that the immune system responds to, but there is a hierarchy as far as which antigen is dominant,” explains study co-lead author Dr. Chih Ming Tsai, a project scientist in the Liu Lab. “Most vaccines are based on the dominant antigen to trigger the strongest possible immune response. But our findings suggest that for SA, the rules are different, and it is more beneficial to target so-called subdominant antigens, which triggered a weak immune response in the first place.”
Researchers are now probing why the natural human immune response to SA is typically ineffective, which could revolutionize not only SA vaccine development but also the approach to other failed vaccines.
“Somehow, SA is able to trick our immune system, and figuring out how will help us improve existing SA vaccines and develop new ones,” concludes Liu. “More broadly, these findings suggest a whole new way of reevaluating failed vaccines, which could have implications well beyond this one bacterium.”
The study is published in the journal Cell Reports Medicine.
You might also be interested in:
