“Tickborne disease” seems almost synonymous with Lyme disease – an illness contracted from blacklegged ticks (deer ticks) infected with the bacteria Borrelia burgdorferi or B. mayonii. Lyme disease may be the most common tickborne disease in the United States, but there’s actually a disturbing smorgasbord of ticks and tickborne bacteria that can cause diseases in the U.S.
Which ticks commonly bite humans?
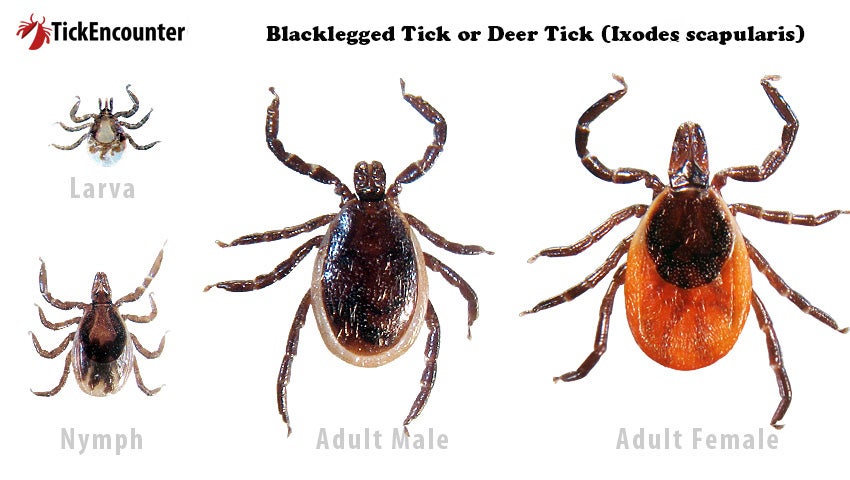
The blacklegged tick (deer tick) is a common sight throughout the Northeast but is also found in the Upper Midwest and mid-Atlantic. It usually bites in the spring, summer, and fall, but may bite in the winter when the temperature is above freezing. It can transmit:
- Borrelia burgdorferi and B. mayonii, which cause Lyme disease
- Anaplasma phagocytophilum, which causes anaplasmosis
- B. miyamotoi, which causes a form of relapsing fever disease
- Ehrlichia muris eauclairensis, which causes ehrlichiosis
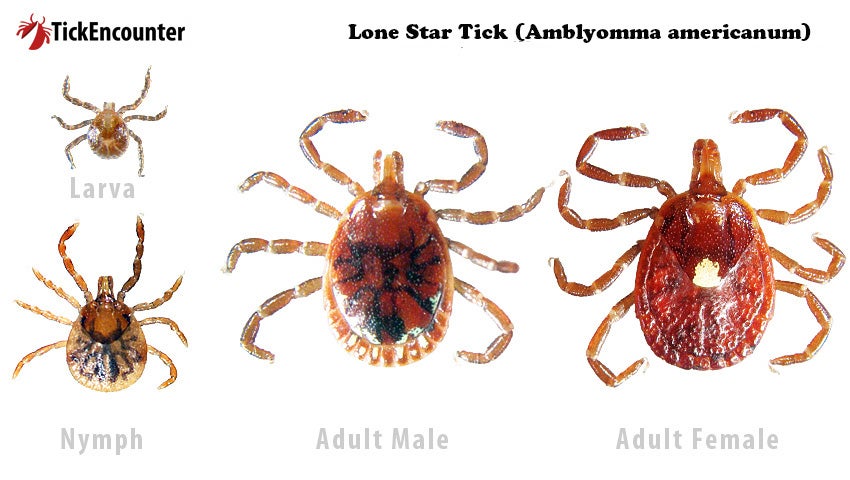
The Lonestar tick lives throughout the eastern United States, but it is more common in the South. It carries quite a few infectious organisms: Ehrlichia chaffeensis and E. ewingii (which cause human ehrlichiosis), Francisella tularensis (tularemia), Heartland virus (Heartland virus disease), Bourbon virus (Bourbon virus disease), and Southern tick-associated rash illness (STARI).
This tick is aggressive, biting frequently from early spring through late fall. The adult female has a white dot or “lone star” on her back. It is the nymph and adult females which usually bite humans.
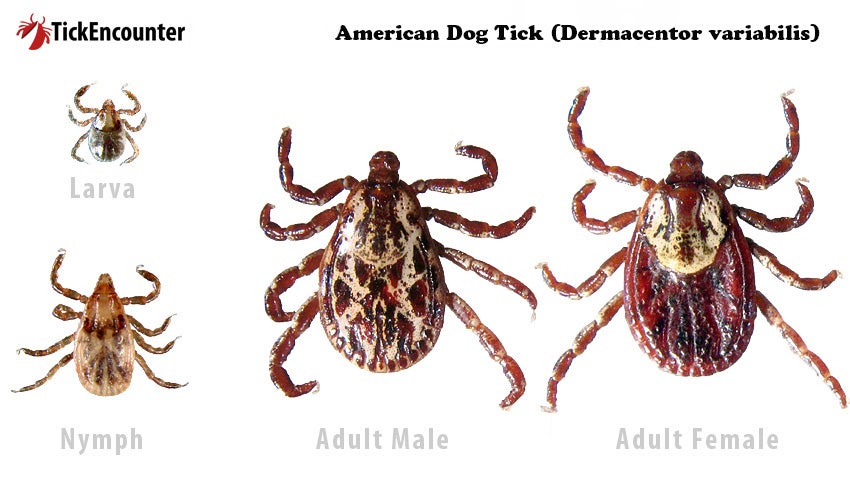
The American dog tick is widely scattered east of the Rocky Mountains. More research is still necessary to understand the role of this species in disease transmission. This tick carries Francisella tularensis (tularemia) and Rickettsia rickettsii (Rocky Mountain spotted fever). Again, the adult females usually do the biting. The greatest risk is during spring and summer.
What other diseases do ticks cause?
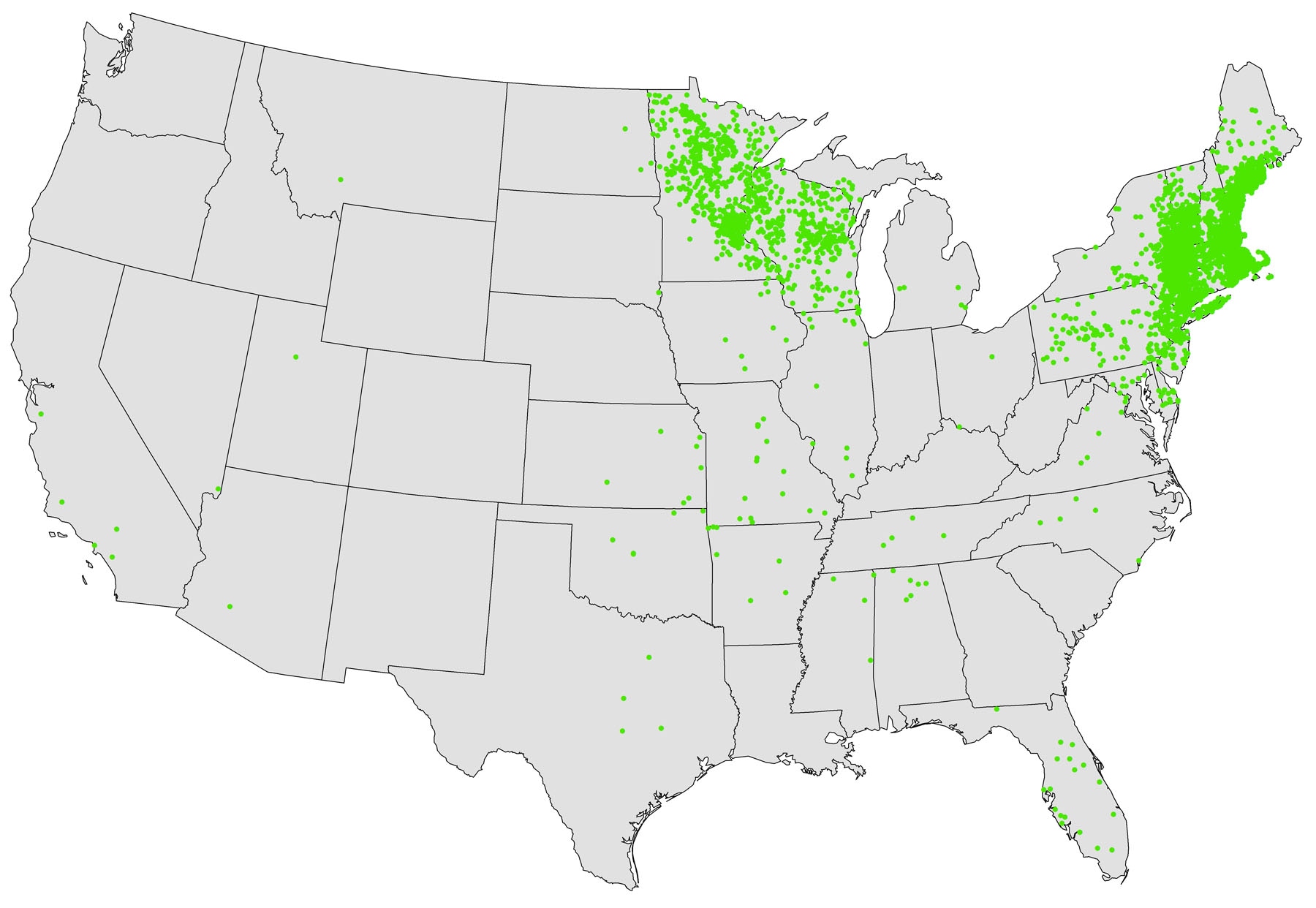
The bacteria Anaplasma phagocytophilum causes anaplasmosis. It is most frequently reported from the Upper Midwest and northeastern United States, the same areas as Lyme disease. The same tick as Lyme disease carries A. phagocytophilum also, so coinfection with burgdorferi (the bacteria that causes Lyme disease) is possible. Patients with both diseases may be sicker, or they may have only a partial response to treatment.
Signs and symptoms appear in five to 14 days. They include fever and chills, severe headache, malaise, muscle aches, and gastrointestinal symptoms (nausea, vomiting, diarrhea, anorexia). There is a rash less than 10 percent of the time. Most people don’t have all the symptoms. Laboratory work confirms the diagnosis. DNA from the organism is found in the blood of an infected person, and special staining will show the organism in skin, tissue, or bone marrow biopsies.
Anaplasmosis, ehrlichiosis, and spotted fever are all treated with the antibiotic doxycycline. When any of these diseases are suspected, treatment should be given immediately. Patients get sicker, faster, when treatment is delayed. The disease can be fatal. Your doctor will usually consult an infectious disease specialist if you are pregnant or allergic to doxycycline.
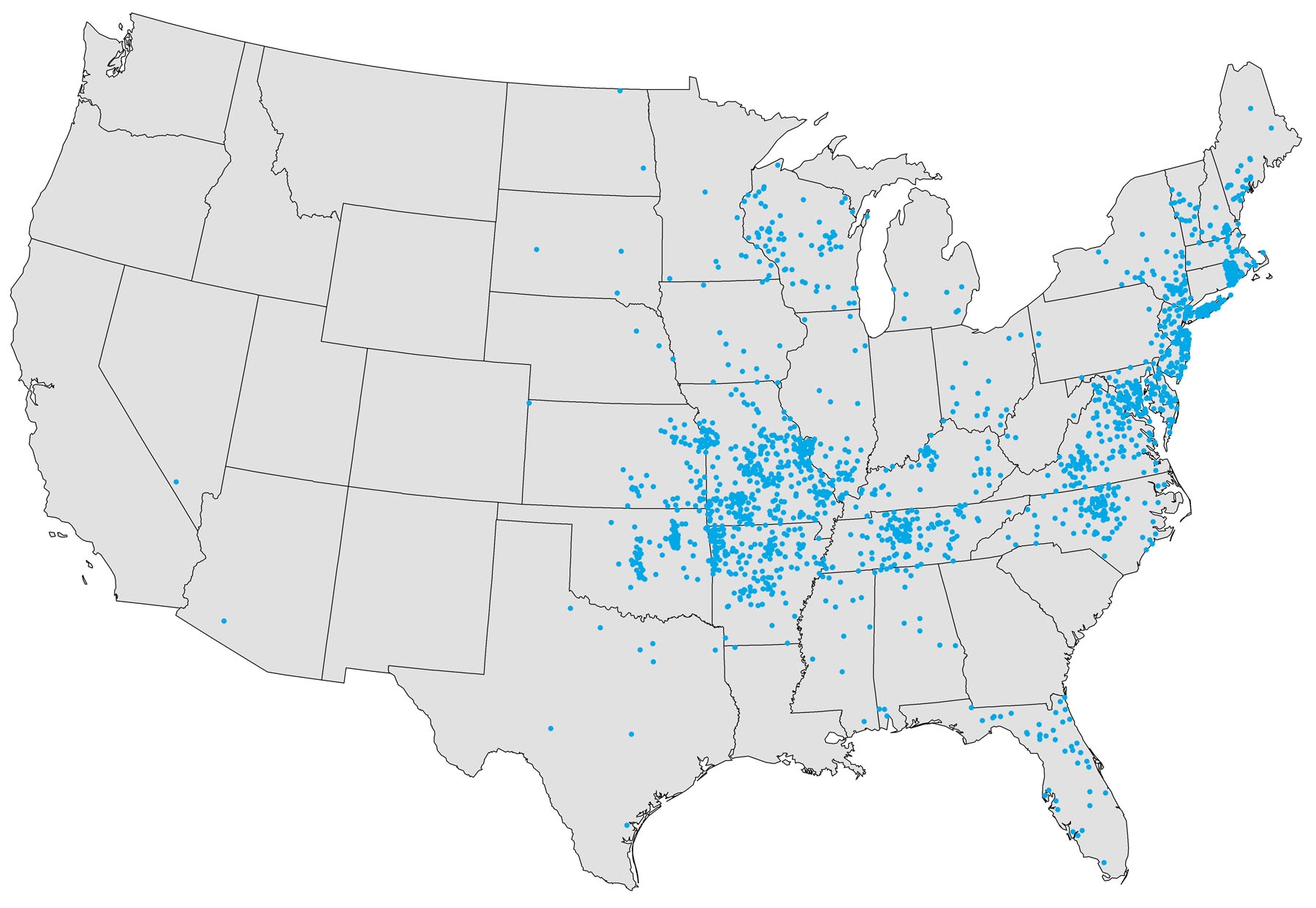
Ehrlichia chaffeensis, Ehrlichia ewingii, Ehrlichia muris eauclairensis are the causes of ehrlichiosis. It is most frequently reported from the southeastern and south-central United States, from the East Coast to Texas. The areas are the same as those in which the lone star tick is distributed. In 2019, Missouri, Arkansas, North Carolina, and New York accounted for about half of all reported cases of E. chaffeensis ehrlichiosis.
Signs and symptoms start to appear in five and 14 days. They include fever and chills, headache, malaise, muscle pain, nausea, vomiting, diarrhea, and anorexia, as well as altered mental status and rash (more common in children.) Few people have all the symptoms. The number and combination of symptoms can vary greatly from person to person.
Bloodwork during the first week of clinical disease shows low white blood cell and platelet counts, as well as anemia. Liver enzyme tests are elevated. DNA is found in the blood, and the organism can be found in skin, tissue, or bone marrow biopsies.
Treatment with doxycycline should begin with the first suspicion of the disease. Delay can be fatal.
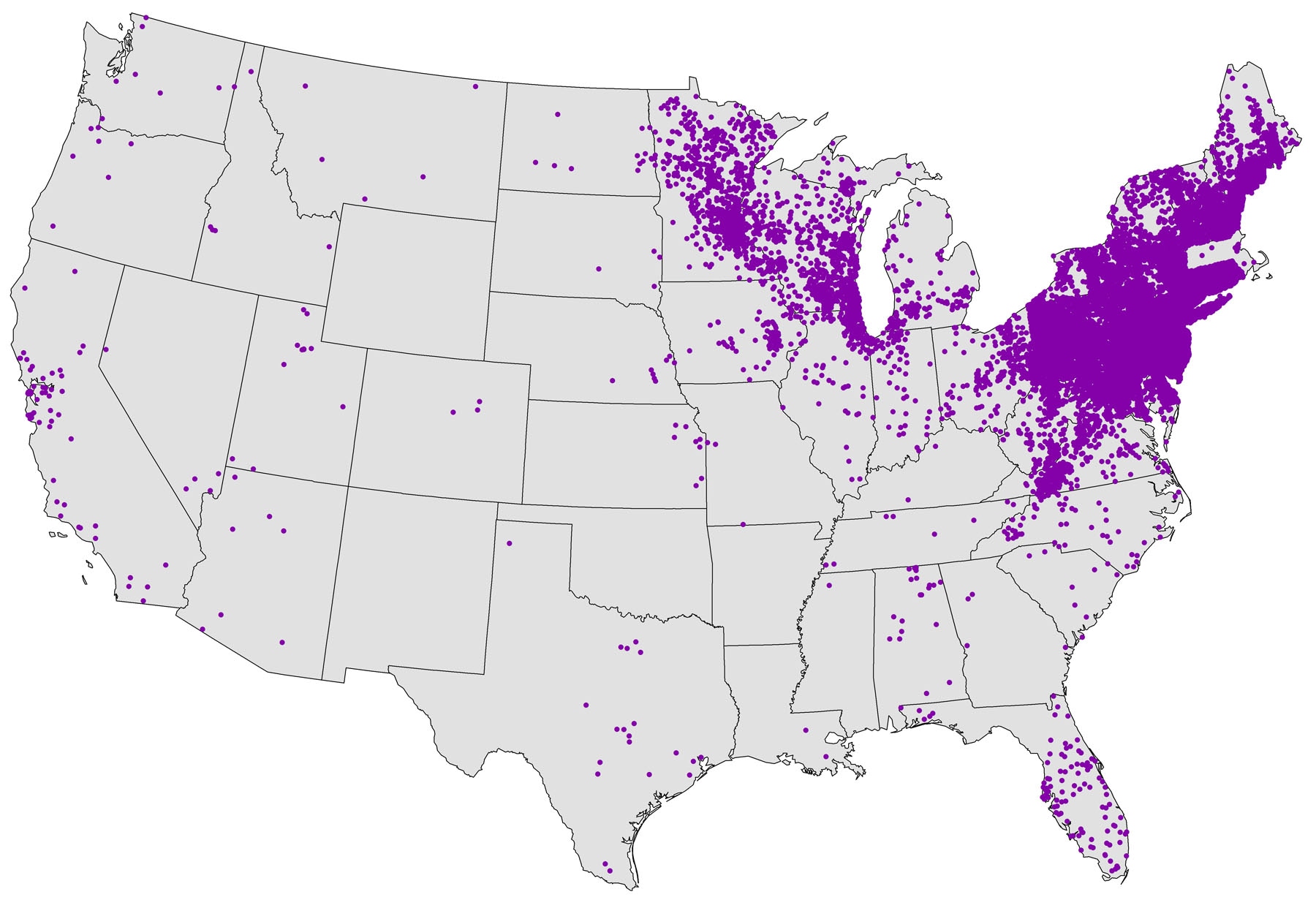
Borrelia burgdorferi and B. mayonii bacteria cause Lyme disease. It is most frequently reported from the upper midwestern, northeastern, and mid-Atlantic states where blacklegged ticks spread the disease. Some cases are reported from northern California, Oregon, and Washington. Connecticut, Delaware, Maine, Maryland, Massachusetts, Minnesota, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, Vermont, Virginia, Washington D.C., West Virginia, and Wisconsin have the highest rates of disease. The affected area is expanding to include neighboring states.
Signs and symptoms appear three to 30 days after a tick bite.
Erythema migrans (EM) is a red ring or homogeneous rash at the site of the tick bite in 70 to 80 percent of infected people. It expands over several days to more than five centimeters in diameter; there may be central clearing resulting in a “bull’s-eye” appearance. It may feel warm but isn’t itchy or painful. Fever, chills, malaise, fatigue, headache, muscle and joint aches, and lymphadenopathy may appear.
Untreated or unnoticed early Lyme disease will spread throughout the body in about 60 percent of patients. Most manifestations will appear in the first few weeks to months of infection, though joint symptoms may be delayed.
People treated with appropriate antibiotics in the early stages of Lyme disease usually recover rapidly and completely. Early diagnosis and proper antibiotic treatment of Lyme disease can help prevent late Lyme disease. Consult an infectious disease specialist regarding individual patient treatment decisions. For treating other manifestations, the CDC offers several tips and recommendations.
Rickettsia rickettsia is the organism which causes what was formerly reported as Rocky Mountain spotted fever (RMSF). Since 2010, RMSF is reported as spotted fever rickettsiosis along with similar diseases like Rickettsia parkeri rickettsiosis. In the eastern, central, and western United States, RMSF is transmitted by the American dog tick, along the U.S.-Mexico border by the brown dog tick, and in the Rocky Mountain states by the Rocky Mountain spotted tick.
Early signs and symptoms appear in one to four days. Without rapid treatment it can be fatal within five days. These early findings are high fever, severe headache, muscle pain, edema around the eyes and backs of the hands, anorexia, nausea, and vomiting. At five days and after, signs and symptoms include brain edema with altered mental status, lung edema with breathing distress, tissue death requiring amputation, and multisystem organ failure.
A rash may appear two to five days after the start of symptoms, but 10 percent of people with the disease never develop a rash. Treatment with antibiotics should begin as soon as RMSF is suspected, even if there is no rash. The early rash consists of small, flat pink spots on the wrists, forearms, and ankles which spreads to the trunk, and sometimes the soles and palms. It is not itchy. The later rash, day six or after consists of tiny red to purple spots (petechiae), which indicate severe disease.
Early laboratory findings include a low platelet count, increased liver enzymes and low blood sodium, but they may be normal.
Antibody tests may be normal through the 10th day of the disease. Antibody tests should not be relied on to confirm the disease. Antibiotic treatment must begin as soon as the disease is suspected.
Doxycycline is the antibiotic of choice for treatment. Delay in treatment can result in severe disease or death.
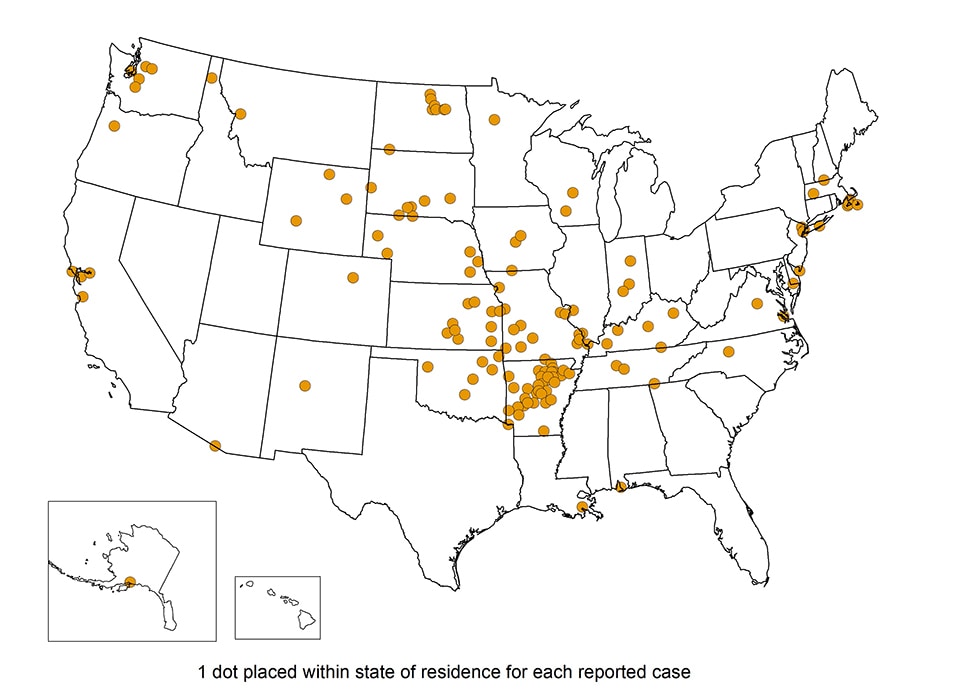
Francisella tularensis is the highly infectious bacterium which causes tularemia. It is spread by deer flies and several species of ticks. It is also spread by infected carcasses or animals (rabbits, rodents), and contaminated food or water. It is most common in the south-central United States, the Great Plains, and Massachusetts.
The incubation period is one to 21 days, but usually three to five days. The signs and symptoms are many, somewhat dependent on the method of infection. Tularemia can be serious or fatal without adequate treatment. Unusual and severe clinical presentations can occur in patients with immunocompromising conditions. The following are common to all forms of the disease:
- Fever, chills
- Headache
- Fatigue
- Anorexia
- Muscle pain
- Chest discomfort, cough
- Sore throat
- Vomiting
- Diarrhea
- Abdominal pain
General laboratory findings include:
- Low sodium
- High white blood cell count
- Low platelet count
- High liver enzymes
- High creatine kinase
- Muscle breakdown products in urine
- Pus in urine without infection
F. tularensis in culture is the best test for diagnosis but can be difficult to obtain because it’s slow and difficult to grow. Blood cultures are often negative.
Antibody tests can confirm the diagnosis when tularemia is suspected but may not be positive until two to three weeks after initial illness.
Treatment should start as soon as the disease is suspected; it should not wait for positive laboratory tests. The antibiotics of choice are gentamicin, ciprofloxacin, and doxycycline. An infectious disease specialist should be consulted in cases in older people, and with underlying health conditions, significant medical history, pregnancy, or allergies.