HANOVER, N.H. — Medicare fraud has rapidly spread across the United States, and researchers at the Dartmouth Geisel School of Medicine have uncovered new insights into this concerning trend. The team examined the characteristics shared by regions where fraudulent Medicare home healthcare billing was most prevalent. These factors included the sharing of patients among multiple agencies, high expenditure rates in specific regions, rapid increases in rates over time, and the presence of a Department of Justice (DOJ) anti-fraud office. The study also found evidence of a peer effect in agency billings, indicating the local sharing of fraudulent practices among agencies.
Home health agencies (HHAs) play a crucial role in providing medical services to Medicare beneficiaries, such as skilled nursing, in their homes. However, fraudulent behaviors have been observed, including unnecessary billing, kickbacks, and sharing of patient IDs by organized criminal organizations.
The research team developed a network analysis tool called a bipartite mixture (BMIX) index, which allowed them to measure the links between patients and HHAs. By analyzing fee-for-service Medicare claims data, they observed a significant increase in home healthcare activity from 2002 to 2009, with expenditures doubling from $14.9 billion to $33.7 billion.
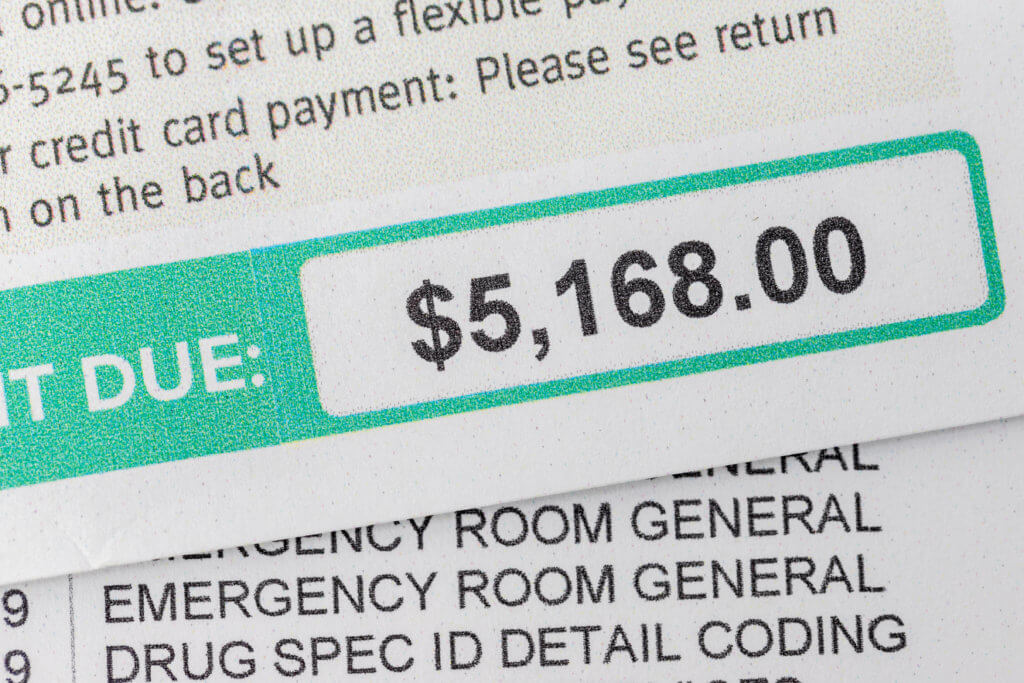
The study revealed that fraudulent behavior was concentrated in specific regions, and these regions were also targeted by DOJ anti-fraud offices. For example, in McAllen, Texas and Miami, Florida, Medicare billing per enrollee increased significantly compared to other regions. The study team developed a theoretical economic model to explain the rapid expansion of fraud and where fraudulent behavior is more likely to occur.
“It more or less makes the argument that if the benefits exceed the risks in the eyes of the perpetrators, then it’s more likely that you’ll see this type of fraudulent behavior—where people are willing to risk conviction, fines, and imprisonment to make larger profits,” explains study lead author James O’Malley, MS, Ph.D., in a university release.
The BMIX index showed promise in predicting excessive billing behavior in HHAs, indicating its potential in machine learning approaches to uncovering Medicare fraud. O’Malley hopes that these methods will be utilized by organizations responsible for policing the healthcare system, allowing for early detection and prosecution of violators to save taxpayer money.
The Dartmouth Institute for Health Policy and Clinical Practice leads the way in studying and advancing disruptive models for healthcare delivery. Researchers say their work includes shared decision-making, the introduction of Accountable Care Organizations, and challenging the notion that more healthcare necessarily equates to better care.
The study is published in the journal Social Science & Medicine.

