NEW YORK — There is so much about the brain we still don’t understand, but a new study has discovered some of the hidden connections that could soon help people suffering from various immune disorders. Researchers from Columbia University’s Zuckerman Institute have discovered that the brain possesses a remarkable ability to detect, amplify, and suppress inflammation in mice. This finding sheds new light on the intricate relationship between the brain and the immune system, potentially paving the way for novel therapies targeting a wide range of autoimmune diseases and inflammatory disorders.
“The brain is the center of our thoughts, emotions, memories and feelings,” says co-first study author Dr. Hao Jin, who started this study as a postdoctoral researcher at Columbia and is now a tenure track investigator at the National Institute of Allergy and Infectious Diseases, in a media release. “Thanks to great advances in circuit tracking and single-cell technology, we now know the brain does far more than that. It is monitoring the function of every system in the body.”
The study, published in the journal Nature, builds upon recent work revealing the importance of the body-brain axis. This vital pathway allows for the exchange of information between various organs and the brain, enabling the brain to monitor and control the body’s biological processes.
To investigate the brain’s potential connections with inflammation and innate immunity, researchers focused on the innate immune system, a defense mechanism shared by all animals. Unlike the adaptive immune system, which remembers previous encounters with pathogens, the innate immune system attacks anything with common traits of germs, allowing for a quicker response to new threats.
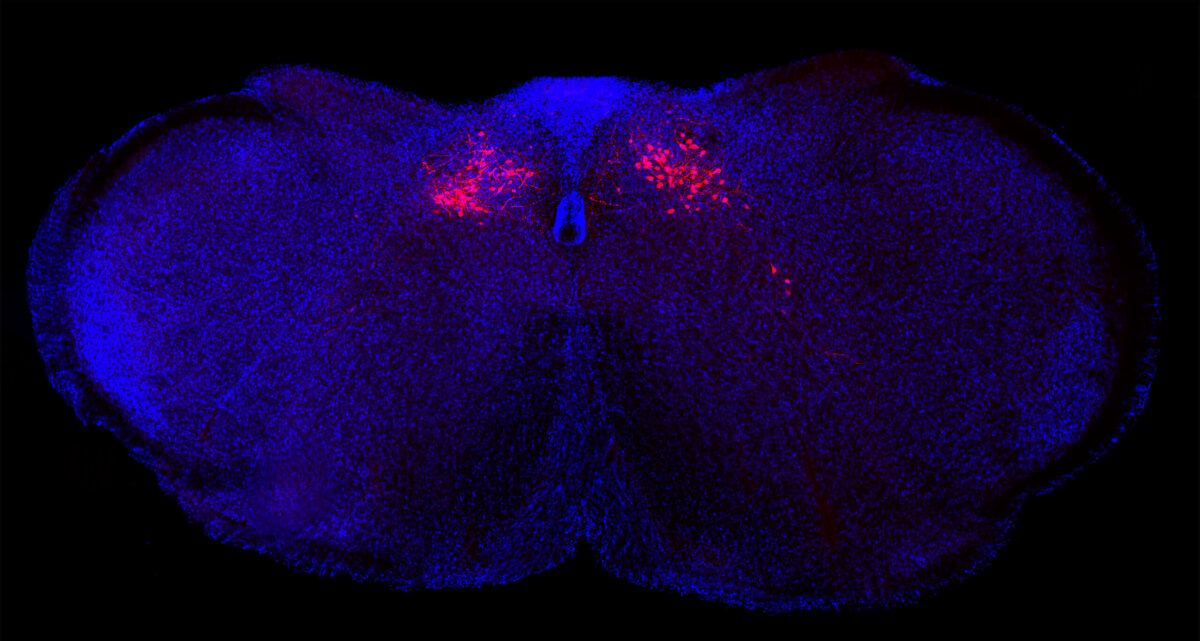
The team discovered that a specific region of the brainstem, known as the caudal nucleus of the solitary tract (cNST), plays a crucial role in regulating inflammatory responses. By chemically suppressing the cNST in mice, the researchers observed an uncontrolled inflammatory response, with levels of pro-inflammatory molecules more than tripling and anti-inflammatory compounds decreasing by roughly two-thirds. Conversely, artificially activating the cNST resulted in a significant reduction in pro-inflammatory molecule levels and a nearly ten-fold increase in anti-inflammatory chemical levels.
“Similar to a thermostat, this newfound brain circuit helps increase or decrease inflammatory responses to keep the body responding in a healthy manner,” explains Dr. Jin. “In retrospect, it makes sense to have a master arbiter controlling this vital response.”
The implications of this discovery extend beyond mice, as previous research involving vagus nerve stimulation in humans suggests similar mechanisms may be at play. The findings also align with long-held beliefs about the mind’s influence on the body.
“A lot of psychosomatic effects could actually be linked to brain circuits telling your body something,” notes Dr. Jin.

By identifying the specific groups of neurons in the vagus nerve and the cNST responsible for detecting and controlling pro- and anti-inflammatory activity, researchers have opened up new avenues for exploring how the brain monitors and modulates body physiology. This breakthrough could lead to the development of innovative therapies for a wide range of autoimmune diseases and inflammatory conditions, such as rheumatoid arthritis, Type 1 diabetes, multiple sclerosis, lupus, inflammatory bowel disease, Crohn’s disease, and even long COVID syndrome.
Autoimmune diseases are estimated to affect approximately one in 10 individuals worldwide, according to a 2023 Lancet study. In the United States alone, the economic burden of autoimmune diseases may exceed $100 billion annually, as reported by the Autoimmune Association. By harnessing the activity of this newly discovered brain circuit, researchers hope to make a significant impact on the lives of those suffering from immune-related disorders.
“This new discovery could provide an exciting therapeutic venue to control inflammation and immunity,” says senior study author Dr. Charles S. Zuker, a principal investigator at Columbia’s Zuckerman Institute and a Howard Hughes Medical Institute investigator.
As research continues to unravel the complexities of the body-brain axis, the potential for groundbreaking treatments targeting the brain’s influence on inflammation and immunity grows increasingly promising.
StudyFinds’ Matt Higgins contributed to this report.
