OAK BROOK, Ill. – Artificial intelligence could do a better job of helping countless women (and even men) at risk for breast cancer. A new study finds AI technology is 25 percent more effective than current online tools at predicting a patient’s risk for the disease. Researchers working with the Radiological Society of North America say the AI systems are more sensitive, making them less likely to miss the most life-threatening cases.
Machine learning algorithms outperform the current methods in predicting the five-year likelihood of the disease. This finding is based on a study of thousands of mammograms.
“Clinical risk models depend on gathering information from different sources, which isn’t always available or collected,” says lead researcher Vignesh Arasu, M.D., Ph.D., a research scientist and practicing radiologist at Kaiser Permanente Northern California. “Recent advances in AI deep learning provide us with the ability to extract hundreds to thousands of additional mammographic features.”
According to the American Cancer Society, doctors will diagnose nearly 300,000 new cases of invasive breast cancer in women this year across the United States. Over 43,000 U.S. women will die from breast cancer in 2023. The average age at the time of a patient’s breast cancer diagnosis is 62.
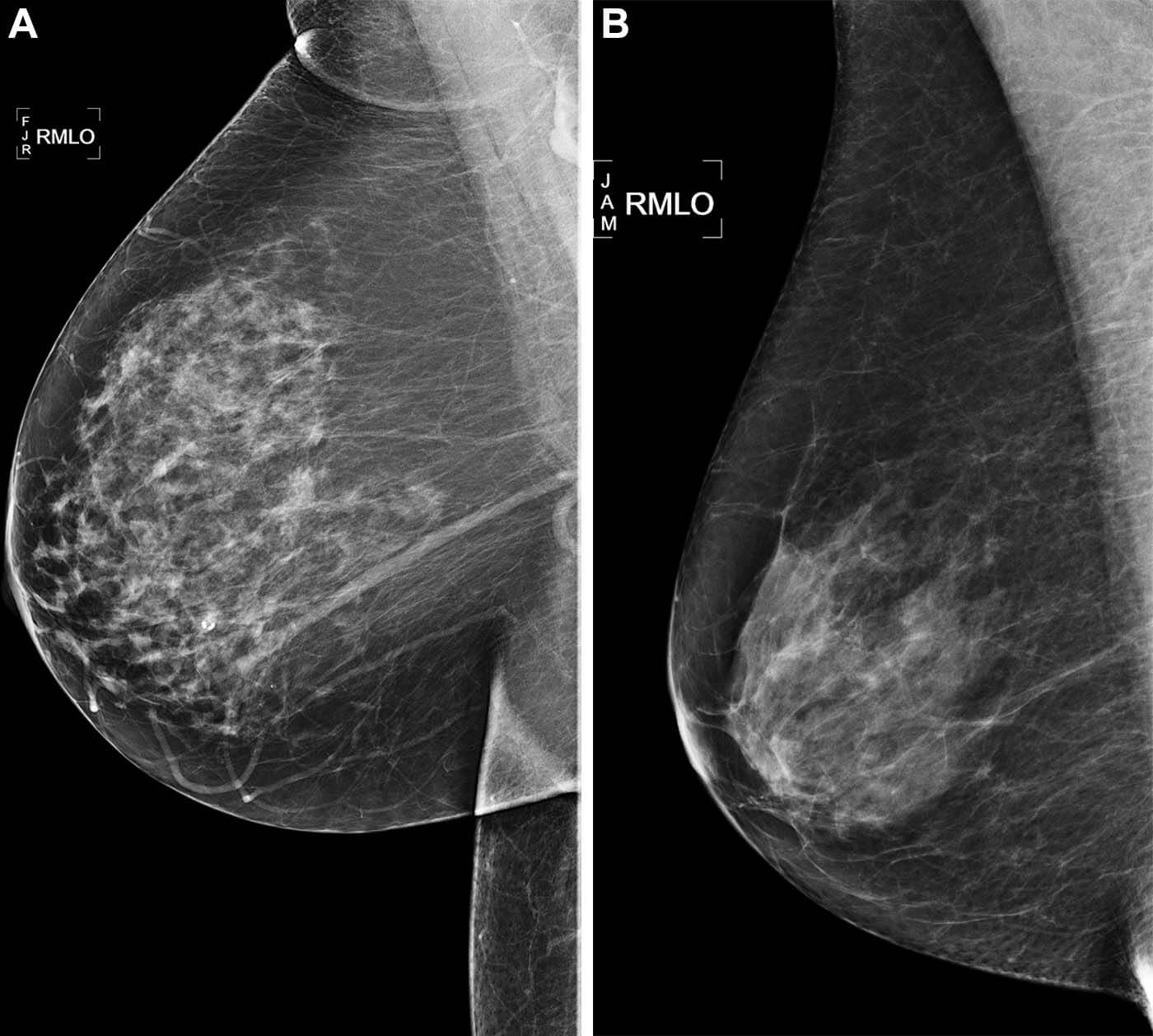
Typically, a woman’s risk is calculated using the BCSC (Breast Cancer Surveillance Consortium). This involves calculations using self-reported information, age, family history of the disease, pregnancy records, and tissue density.
Some algorithms have excelled at identifying aggressive tumors. For instance, when evaluating those at the highest risk, AI predicted up to 28 percent of cancers compared to 21 percent with BCSC.
“All five AI algorithms performed better than the BCSC risk model for predicting breast cancer risk at 0 to 5 years,” Dr. Arasu says in a media release. “This strong predictive performance over the five-year period suggests AI is identifying both missed cancers and breast tissue features that help predict future cancer development. Something in mammograms allows us to track breast cancer risk. This is the ‘black box’ of AI.”
Dr. Arasu’s team analyzed a random sample of over 18,000 women who underwent mammograms at the clinic in 2016. About a quarter of these women were diagnosed with tumors within the subsequent five years.
Even AI algorithms that were only trained for three months were effective when no cancer was clinically detected during screening. The integration of these algorithms with BCSC further improved the results.
“We’re looking for an accurate, efficient and scalable means of understanding a women’s breast cancer risk,” Dr. Arasu continues. “Mammography-based AI risk models provide practical advantages over traditional clinical risk models because they use a single data source: the mammogram itself.”
Some institutions are already using AI to assist radiologists in detecting cancer on mammograms. A person’s future risk score, which takes only seconds for AI to generate, could be integrated into the radiology report shared with the patient and their physician.
“AI for cancer risk prediction offers us the opportunity to individualize every woman’s care, which isn’t systematically available,” Dr. Arasu concludes. “It’s a tool that could help us provide personalized, precision medicine on a national level.”
The study is published in the journal Radiology.
You might also be interested in:
- Women working with X-rays need more protection to prevent breast cancer, study warns
- Common dietary supplement boosts effectiveness of treatment for drug-resistant breast cancer tumors
- AI program accurately predicts how long cancer patients will survive by reading doctors’ notes
South West News Service writer Mark Waghorn contributed to this report.