TORONTO — A groundbreaking new imaging technique could soon revolutionize breast cancer diagnosis by offering more accurate and less invasive alternatives, especially for women with dense breast tissue, researchers say.
The cutting-edge screening method, referred to as low-dose positron emission mammography (PEM), produces significantly fewer false-positive results compared to MRI scans and is believed to be more comfortable than traditional mammogram screenings.
Traditional mammograms often struggle to accurately diagnose women with dense breast tissue—a challenge not faced by PEM scans. Individuals with dense breasts are at an increased risk for cancer, though the reasons remain unclear.
Although mammography is an effective tool for the early detection of breast cancer, its accuracy diminishes in patients with dense breast tissue. Dense breast tissue, characterized by higher amounts of glandular and fibrous connective tissue and lower amounts of fatty tissue, complicates cancer detection efforts.
Given that nearly half of the screening population possesses dense breasts, many require additional imaging, often through MRI scans, following a mammogram.
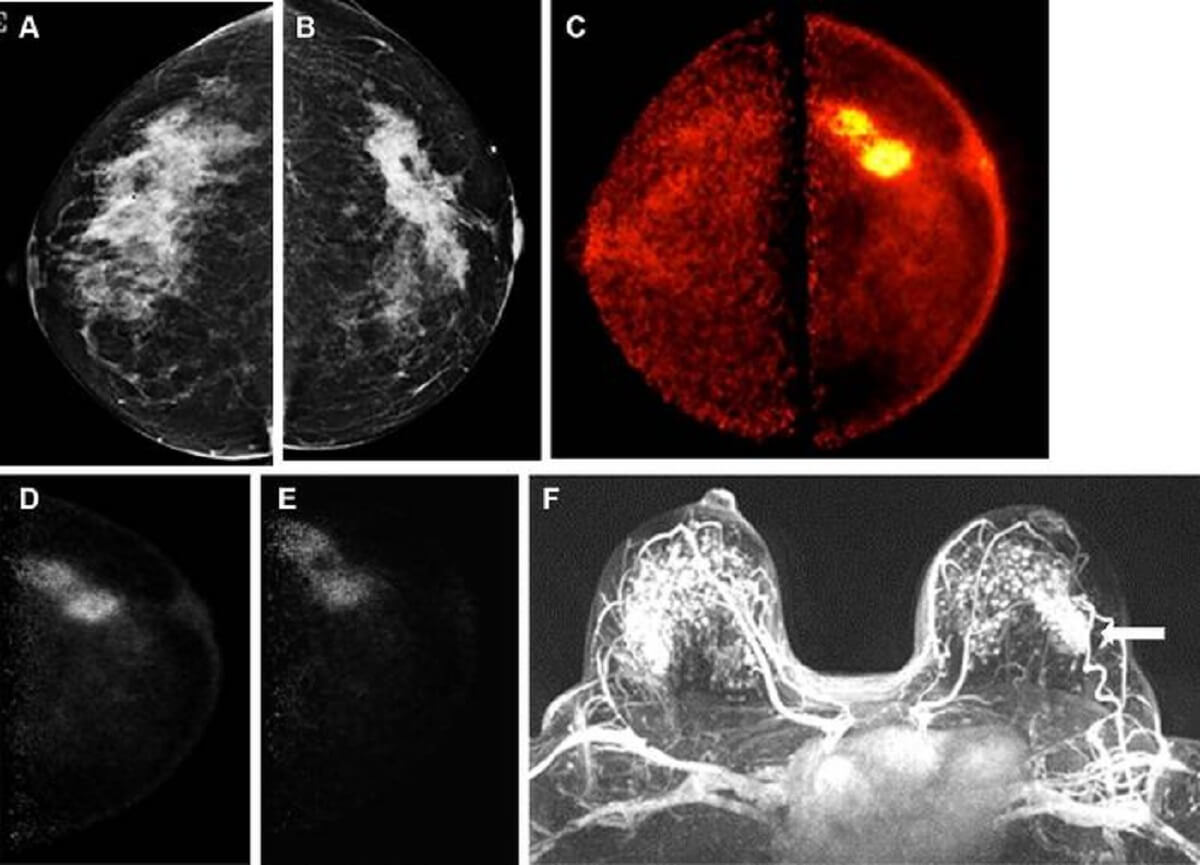
In the study led by the University of Toronto, 25 women with an average age of 52, recently diagnosed with breast cancer, underwent low-dose PEM after receiving an injection of the radiotracer fluorine 18-labeled fluorodeoxyglucose (18F-FDG).
Two breast radiologists reviewed the PEM images captured one and four hours post-injection, correlating their observations with laboratory results.
The research reveals that PEM matched the performance of MRI scans in identifying 24 out of 25 invasive cancers (96%), with a significantly lower false-positive rate of 16%, compared to 62% for MRIs.
Besides its impressive sensitivity and accuracy, PEM could also reduce healthcare expenses by preventing the additional diagnostic procedures often necessitated by less accurate MRIs.
This technology might also offer a more comfortable experience than mammograms by avoiding breast compression while delivering a radiation dose similar to traditional mammography.
“The combination of high sensitivity, reduced false-positive rates, cost-effectiveness, acceptable radiation levels without compression, and effectiveness regardless of breast density makes this new imaging technique a potentially transformative development in early breast cancer detection,” says Dr. Vivianne Freitas, an assistant professor at the University of Toronto and the study’s lead author, in a Radiological Society of North America media release. “It promises to enhance or even refine current imaging practices, representing a significant leap forward in breast cancer care. Specifically, its efficacy in dense breast tissue addresses a notable limitation of mammography, offering an alternative for patients at high risk, including those who are claustrophobic or have contraindications for MRI.”
PEM could also aid in clarifying ambiguous mammogram results, evaluating chemotherapy responses, and assessing the disease’s extent in newly diagnosed cases, including the potential involvement of the contralateral breast.
The researchers are further exploring PEM’s capacity to lower the high incidence of false-positives associated with MRI scans, with additional research needed to fully understand low-dose PEM’s clinical role and effectiveness. If successful, PEM could significantly alleviate the emotional and psychological strain linked to false-positives, reducing the number of unnecessary biopsies and treatments.
“While the complete integration of this imaging method into clinical practices awaits confirmation, the initial results are promising, especially in demonstrating its ability to detect invasive breast cancer with low doses of fluorine-18-labeled FDG,” Dr. Freitas concludes. “This signifies a crucial initial step towards its potential adoption in clinical settings.”
The study is published in the journal Radiology: Imaging Cancer.
SWNS writer James Gamble contributed to this report.
This is a great breakthrough. But too late for me. I was told I had dense breasts for decades of faithful yearly mammograms but no suggested follow up. The tumor was large but could not be seen on mammogram or ultrasound. Only MRI and only because it had gone into two nearby lymph nodes that did show up on the mammogram. I opted for a partial mastectomy but wish I had gone for full mastectomy of the affected side and reconstruction of both breasts My latest MRI showed no evidence of disease.