Cancer can be a terrifying word, but knowledge can be a powerful weapon in stopping or preventing the disease.
Screening and early detection of cancer go hand in hand. Screening refers to tests and exams used to find a disease in people who do not have any symptoms. Early detection means finding and diagnosing a disease, ideally before symptoms appear.
Cancers found by screening are more likely to be smaller and less likely to have spread outside the area in which the tumor formed. The size of a tumor and how far it has spread outside its origin are two of the most crucial factors in predicting the prognosis (the possible outcome) for a person with a disease.
Through rigorous research, health officials have created guidelines for how and when to screen for some of the most common cancers. As new knowledge about cancer is discovered, screening recommendations are adjusted. One size does not fit all with cancer screening. Screening options should always be discussed with your personal healthcare provider.
Unfortunately, not all the information out there about cancer screenings and detecting the disease early is right. So, here are 10 important notes to remember when it comes to screening for cancer.
1. Women with an average risk for breast cancer do NOT need to begin annual mammograms at age 40.
Here are the current recommendations:
- Women between 40 and 44 should have the option to start screening with a mammogram every year.
- Women 45 to 54 should get mammograms annually.
- Women 55 and older can switch to a mammogram every other year, or they can choose to continue yearly mammograms.
- Screening should continue if a woman is in good health and is expected to live at least 10 more years.
For screening purposes, a woman has an “average risk” if she doesn’t have a personal history of breast cancer, a strong family history of breast cancer, or a genetic mutation known to increase the risk of breast cancer (such as in a BRCA gene), and has not had chest radiation therapy before the age of 30.

2. Research is unclear on the benefits of regular physical breast exams done by a health professional or by women themselves.
However, health professionals strongly encourage monthly breast self-exams. There are reasons for this. Women need to know what their normal breast tissue feels like. Breast tissue tends to feel lumpy, bumpy, and cord-like in places. Every woman has unique-feeling breasts. It is by knowing how her own breast tissue feels that she knows when she feels something different. Women should report a difference to a healthcare provider without delay.
3. Women with dense breast tissue are more likely to develop breast cancer.
Breast density is a measure of how much fibrous and glandular tissue (also known as fibroglandular tissue) there is in a breast, compared to fat tissue. The size and firmness of breasts are not related to density. Breast density is important because:
- Women who have dense breast tissue have a higher risk of breast cancer compared to women with less dense breast tissue. Why is still unclear. Scientists speculate that dense breast tissue has more cells that can develop into abnormal cells.
- Dense breast tissue makes it more difficult for doctors who are X-ray specialists to see cancer on mammograms. Dense breast tissue looks white on a mammogram. Breast masses and cancers can also look white, so the dense tissue can make it harder to see them. Fatty tissue in a breast looks almost black on a mammogram, so it is easier to see a tumor that looks white.

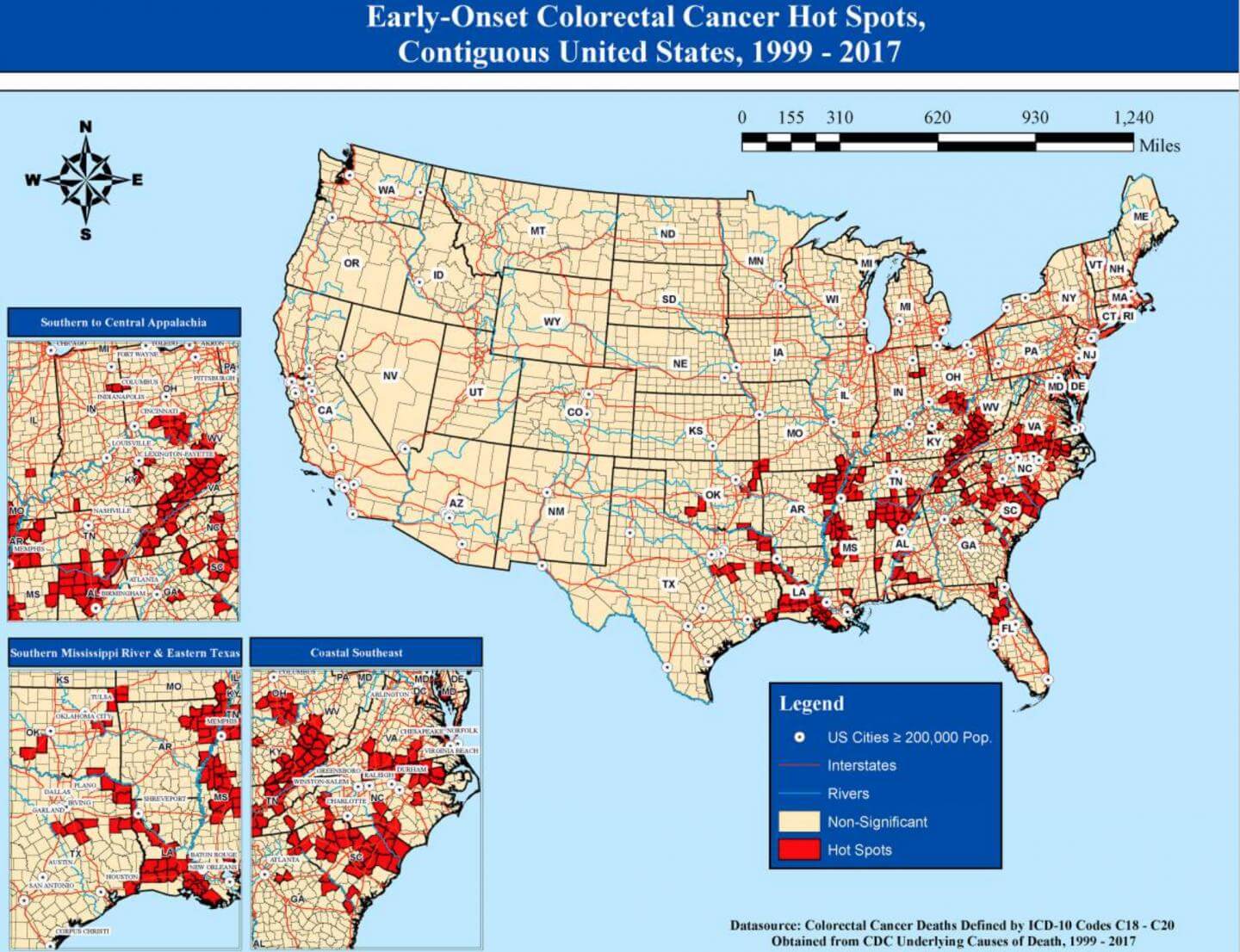
4. People who are at average risk for colorectal cancer should NOT wait until age 50 to begin screening.
More cases of colorectal cancer are being diagnosed at increasingly younger ages. For that reason, the current recommendations include:
- Age 45 is when screening for colorectal cancer, with average risk, should begin, through age 75. People with a family history of colorectal cancer should begin screening 10 years younger than their relative was diagnosed.
- At ages 76 through 85, screening is based on a person’s preferences, life expectancy, overall health, and prior screening history.
- People older than 85 should stop being screened for colorectal cancer.
5. Screening tests for colorectal cancer include either stool testing or visualization of the colon and rectum.
The type of screening done should be a mutual decision between you and your healthcare provider. Stool-based tests include:
- Highly sensitive fecal immunochemical test (FIT) every year
- Highly sensitive guaiac-based fecal occult blood test (gFOBT) every year
- Multi-targeted stool DNA test (mt-sDNA) every 3 years
Visual (structural) exams of the colon and rectum include:
- Colonoscopy every 10 years
- CT colonography (virtual colonoscopy) every 5 years
- Flexible sigmoidoscopy (FSIG) every 5 years
6. A 50-year-old smoker should start getting annual chest CT scans to screen for lung cancer.
For example, a 50-year-old man who has smoked one pack of cigarettes per day since age 20 should start getting annual CT scans of his chest to screen for lung cancer. Yearly screening for lung cancer with a low-dose computed tomography (LDCT) scan is recommended for people between 50 and 80 who smoke or who used to smoke and who have at least a “20 pack-year” history of smoking.
- A pack-year is equal to smoking one pack per day for a year.
A patient should discuss the risks and benefits of screening with their healthcare provider. Age is a factor in the decision. The presence of some chronic diseases may make it unnecessary to screen if the chronic disease limits their lifespan. If a patient is not well enough to tolerate treatments (radiation, chemotherapy, surgery), there is less necessity to screen. People who still smoke should be counseled about quitting and given resources to help them quit.
7. Even 30 years after quitting smoking, a person’s risk for lung cancer is NOT the same as someone who never smoked.
For example, let’s look at a 60-year-old woman who smoked two packs of cigarettes per day from age 15 to 30 and then quit smoking.
This woman’s risk for lung cancer is less when compared to a person who is still smoking. Her risk, however, is still that of a person with a 30-pack-year history of smoking.
The years since quitting (YSQ) are not accompanied by a declining risk for cancer – there is no “undoing” of the damage or lessening of risk conferred by time.
This new understanding of lung cancer risk means that former smokers need screening according to their smoking history, not their status as a non-smoker. If you have a history greater than 20-pack-years, discuss screening with your healthcare provider, who may not be aware of your elevated risk for lung cancer if they know you as a nonsmoker.

8. A transgender adult, assigned female at birth, should still be screened for cervical cancer.
Regardless of whether this person is now living as a man and looks forward to surgical alteration, their assigned gender at birth still matters from a health perspective. Screening for cervical cancer:
- Should start at age 25 for anyone with a cervix, including transgender men born as a female. The exception is those who have had their original reproductive anatomy surgically removed. The screening should be done every five years with a primary human papillomavirus (HPV) test. Some types of HPV are known to cause changes in the cells in the cervix, which can lead to cervical cancer. A primary HPV test is one that is used alone. An alternative is a Pap smear every three years.
- At age 65, screening may be discontinued if all previous tests were negative for abnormal changes in the cells of the cervix or if the cervix has been surgically removed, such as by hysterectomy.
9. An elevated prostate-specific antigen (PSA) blood test DOES NOT mean that you have a type of prostate cancer that will respond well to treatment.
Testing, diagnosis, and management of prostate cancer are full of uncertainties. That’s why it’s important to have a thorough discussion with your doctor about what is known and unknown about prostate cancer and the relative usefulness of testing.
Testing will find prostate cancer earlier than if no testing is done. Testing for prostate cancer is performed with the prostate-specific antigen (PSA) blood test with or without a rectal exam. Some men with an elevated PSA level in their blood may not have prostate cancer. Some men with prostate cancer will have a PSA level that is not elevated.
Some men who have cancer may not need to be treated right away. For many men, the progression of the disease is slow, and treatments are not without side-effects. These men need to be watched closely to see whether the cancer changes or grows. Treatments for prostate cancer can lead to side-effects. There can be problems with passing urine, problems with bowels, and/or problems having sex. For some men, these problems are mild and temporary. In other men, these problems are permanent.
When testing finds prostate cancer, some men will have the type of prostate cancer that progresses rapidly and may end in death. It is often not clear which men will have the type of prostate cancer that is not likely to affect their health. Some men will do well with treatment, but some men do well with no treatment. There is no way to know the course of an individual’s disease and treatment.
Before testing, ask yourself if it is important to you to know whether you have the disease when no one can predict the prognosis (outcome). Would you want treatment, knowing that you may not benefit from it and may experience side-effects that lessen your quality of life? These questions are important to discuss with your doctor.

10. You DO NOT need to screen for cancer of the endometrium 5 years after menopause.
There is no screening test for endometrial cancer (the lining of the uterus). The best way to find endometrial cancer when it’s small (at an early stage) is to see a healthcare provider if you have any signs and symptoms of endometrial cancer, such as abnormal vaginal bleeding or discharge that’s getting worse, occurring between periods, or happening after menopause. Early detection improves the chances that the cancer will be treated successfully.
Most women with endometrial cancer have abnormal vaginal bleeding. Still, some endometrial cancers may reach an advanced stage before causing signs and symptoms. This means the cancer is big and may have spread before it causes any problems that are noticed.
The American Cancer Society recommends that, at menopause, all women should be told about the risks and symptoms of endometrial cancer and strongly encouraged to report any vaginal bleeding, discharge, or spotting to their doctor. A pelvic exam can find some cancers, including some advanced uterine cancers, but it is not particularly useful for finding early endometrial cancers.
The ACS also recommends that women at increased risk for endometrial cancer be told of their risk and be advised to see their doctor whenever they have any abnormal vaginal bleeding. This includes women whose risk is increased due to age, late menopause, never giving birth, infertility, obesity, diabetes, high blood pressure, estrogen treatment, or tamoxifen therapy.
You might also be interested in:
- 5 Worrying Breast Conditions That Are Not Cancer
- 9 noticeable signs of cancer to look out for
- Colorectal cancer screening age lowered to 45 as cases skyrocket among younger adults

