HOUSTON — Scientists are warning of a rising threat to public health in the United States. A recent study raises concerns about Candida auris, a fungal pathogen that’s resistant to many vital medications. Researchers from bioMérieux Inc. have identified a significant increase in the detection of this potentially deadly yeast in blood cultures, indicating a worrying trend in antimicrobial resistance.
Candida auris is not just any fungus; it’s an emerging pathogen known for its resistance to many antimicrobial agents, which are drugs used to treat infections. This resistance makes it particularly dangerous and hard to eliminate. According to the study, there was a notable rise in the detection of C. auris from an average rate of 0.014% before October 2022 to 0.057% after October 2022.
The findings, first presented earlier this year during an annual meeting of the American Society for Microbiology, are based on a retrospective analysis. This means the researchers looked back at existing data, in this case, blood cultures from July 2020 to March 2023, to understand the changes in infection rates.
The researchers used two advanced tools for their study: the BIOFIRE BCID2 blood culture identification panel and the BIOFIRE Syndromic Trends (TREND) surveillance network. The BCID2 panel is a test that can identify 43 different targets, including C. auris, in blood samples. The TREND network is a cloud-based system that captures anonymized patient results from over 100,000 positive blood cultures almost immediately, allowing for near real-time tracking of infection trends.
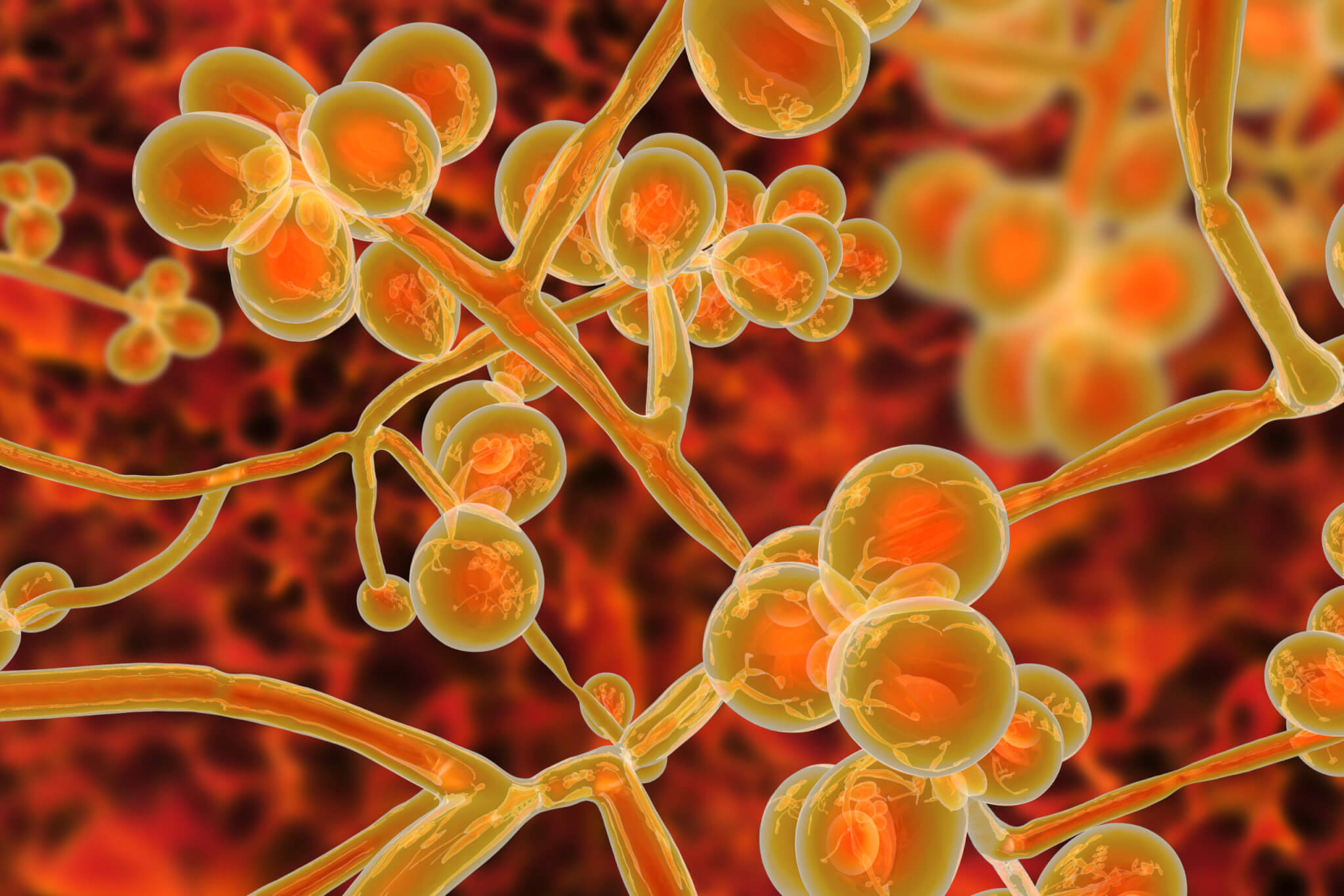
What makes C. auris particularly concerning is its high resistance to disinfectants and multiple antibiotics, with about 50% of isolates exhibiting this resistance. This contributes to high mortality rates when the organism establishes itself in the bloodstream. The pathogen was first detected in the U.S. in 2016, and by 2021, its infection rate had increased by 95%. The recent bioMérieux study found that bloodstream infections caused by C. auris in 2023 were significantly higher compared to previous years.
Tristan T. Timbook, the Director of Health Economics Outcomes Research at bioMérieux, emphasized the importance of public health interventions to combat these challenges. “We need to continue working together with the Centers for Disease Control and Prevention to protect our communities from this dangerous Candida auris that is resistant to many medicines,” he says in a statement. “The near real-time surveillance provided by TREND and the BIOFIRE BCID2 panel represent important tools for monitoring trends in C. auris infection.”
This study underscores the need for ongoing vigilance and advanced monitoring techniques to track and combat the spread of antimicrobial-resistant pathogens like C. auris, which pose a significant threat to community health. Experts say we should follow the guidance provided by the Centers for Disease Control and Prevention and practice good hygiene, such as washing our hands regularly and keeping our surroundings clean. It’s also crucial to be aware of any symptoms, such as fever or feeling unwell, and seek medical help if needed.
How are people being infected with C. auris?
Typically, Candida auris spreads to other humans most often in healthcare settings:
1. Contact with contaminated surfaces or equipment: This is the most common way C. auris spreads. The fungus can live on surfaces for weeks, and people can pick it up by touching contaminated surfaces and then touching their face or a wound. This can happen in hospitals, nursing homes, and other healthcare facilities.
2. Contact with infected or colonized patients: C. auris can also spread from person to person through direct contact with infected or colonized individuals. This can happen through skin-to-skin contact, or through contact with body fluids such as saliva or pus.
Here’s a breakdown of the different ways C. auris infection can occur:
-
Healthcare settings: This is where most cases occur, with outbreaks often reported. The fungus thrives on medical equipment, surfaces, and even the hands of healthcare workers who haven’t properly decontaminated. Patients with weakened immune systems or open wounds are particularly vulnerable.
-
Direct contact: Sharing personal items like towels or razors with an infected person, or coming into close contact with their skin, can transmit the fungus.
-
Environmental exposure: Though less common, C. auris has been found in some water sources and on surfaces in public places like gyms or locker rooms. While direct transmission from these sources is rare, it’s crucial to maintain good hygiene practices, especially if you have risk factors.
It’s important to remember that everyone can take steps to prevent the spread of C. auris:
-
Healthcare workers: Rigorous hand hygiene, thorough disinfection of equipment and surfaces, and following isolation protocols are essential.
-
Patients: If you’re in a healthcare setting, ask about their C. auris precautions and practice good hygiene yourself.
-
General public: Frequent handwashing, avoiding sharing personal items, and being mindful of hygiene in public spaces can help minimize the risk.
The symptoms can vary depending on where the infection is located. However, some of the most common symptoms of C. auris infection include:
- Fever and chills: This is a general sign of infection, and it can be accompanied by other symptoms such as sweating, fatigue, and headache.
- Pain, pressure, or feeling of fullness in the ear: This is a symptom of a C. auris ear infection.
- Drainage from the ear: This can be clear, yellow, or green, and it may have a foul odor.
- Hearing loss: This can be temporary or permanent, and it may be caused by the infection itself or by damage to the eardrum.
- Redness, swelling, or warmth around the ear: This is a sign of inflammation, which is the body’s response to infection.
It’s important to note that not everyone who has C. auris will experience all of these symptoms, and some people may not have any symptoms at all. Additionally, these symptoms can also be caused by other types of ear infections, so it’s important to see a doctor for diagnosis. If you are concerned that you may have a C. auris infection, please see a doctor right away. Early diagnosis and treatment is important for preventing serious complications.

I’m not sure I can trust a source that lumps bacteria, yeast, and fungus together as if they are the same types of organisms