CAMBRIDGE, United Kingdom — A chemical imbalance detected in the brains of those suffering from obsessive-compulsive disorder (OCD) may explain what causes this sometimes-debilitating condition, potentially paving the way for improved treatments. Scientists utilized an advanced MRI scanner to examine the brains of individuals diagnosed with OCD, identifying an imbalance between two neurochemicals in a region crucial for habits and decision-making.
Conducted by researchers at the University of Cambridge, the study also revealed elevated levels of one of the same neurochemicals in individuals who exhibit compulsive behavior without having OCD.
The neuroscientists who spearheaded the study described this finding as a “significant part of the puzzle” in understanding OCD. They utilized a high-powered 7-Tesla Magnetic Resonance Spectroscopy (MRS) scanner, one of only seven in the United Kingdom, located at the Wolfson Brain Imaging Centre at Cambridge. The team scanned the brains of 31 clinically diagnosed OCD sufferers and 30 healthy volunteers as a control group.
OCD is a chronic disorder characterized by uncontrollable, recurring thoughts, known as obsessions, and repetitive behaviors or compulsions. Severe cases can significantly disrupt work performance, relationships, and possibly lead to social isolation. In extreme instances, these behaviors can even provoke suicidal thoughts.
As part of their research, the team also administered tests and questionnaires to all participants to measure obsessive-compulsive and habitual tendencies.
“We tested whether people were more prone to repeating the same responses, like a habit, or adapting their behavior to better pursue goals,” says Professor Trevor Robbins, a senior author of the study from Cambridge’s Department of Psychology, in a university release. “Compulsions and habits are not the same, but impaired regulation of habits can be the basis of compulsions and shift people away from their goal-directed behavior.”
Scroll down to see a list of 7 treatments for OCD
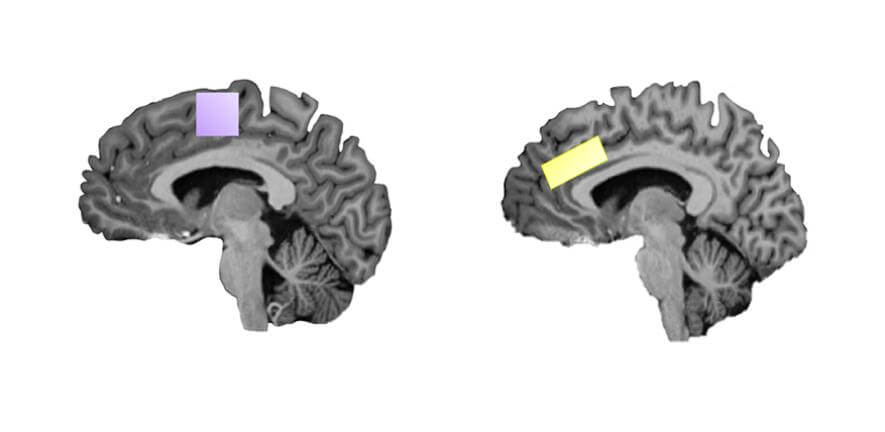
The scientists measured the levels of glutamate and GABA, two significant neurotransmitters, in regions of the cerebral cortex, the outermost and most developed part of the human brain. Glutamate is an “excitatory” neurochemical that facilitates the transmission of information throughout brain networks, while GABA is an “inhibitory” neurotransmitter that counters glutamate by reducing neural excitability, thus creating a balance.
The study finds individuals with OCD had elevated levels of the excitatory neurochemical glutamate and reduced levels of the balancing agent GABA in the anterior cingulate cortex compared to individuals without OCD.
Additionally, the study reveals a correlation between the severity of OCD symptoms and a predisposition towards habitual and compulsive behavior with higher glutamate levels in another brain region, the supplementary motor area. This held true for both OCD patients and healthy participants with milder compulsive tendencies.
The affected brain areas play crucial roles in deciding the balance between our conscious goals and more automatic habits. The research suggests that compulsions “emerge from a dysregulated brain system for controlling habits,” according to the study’s authors.
“Understanding OCD is a critical question for psychiatry. Symptoms of intrusive thoughts and repetitive rituals can confine patients to their homes for months. We have now definitively detected changes in these key neurotransmitters in individuals with OCD,” comments Prof. Robbins. “An excess of glutamate and a reduction of GABA disrupt the neural circuitry in key regions of the brain affected by OCD.”
Presynaptic receptors control the release of neurotransmitter chemicals in a nerve cell. Current OCD treatments are limited. While some patients with milder symptoms benefit from antidepressants, options are scarce for those with severe symptoms.
“Our findings are a major piece of the puzzle for understanding the mechanisms behind OCD. The results suggest new strategies for medication in OCD based on available drugs that regulate glutamate. In particular, drugs that inhibit presynaptic glutamate receptors,” explains Prof. Robbins.
The study’s results could guide future treatment therapies, including medication and non-invasive “magnetic stimulation” through the scalp, which has shown promise in treating OCD.
“Some treatments already target glutamate imbalance in a roundabout way. Now we have the evidence for why certain approaches seem to have some beneficial effects,” says Dr. Marjan Biria, another lead author of the study, who conducted the work in Robbins’ Cambridge lab.
How can patients treat obsessive-compulsive disorder?
Treatment for OCD often involves a combination of medication and psychotherapy. Here’s a list of common treatments:
- Cognitive Behavioral Therapy (CBT): This is a type of psychotherapy that is often very effective for OCD. Specifically, a form of CBT known as Exposure and Response Prevention (ERP) is considered the gold standard treatment. ERP involves gradual exposure to situations that trigger obsessions and learning to resist the accompanying urge to perform compulsive behaviors.
- Medications: Certain types of psychiatric medications are often used to manage OCD symptoms. These include Selective Serotonin Reuptake Inhibitors (SSRIs). These are a class of drugs that increase the amount of serotonin in the brain, which can help reduce OCD symptoms. Examples include fluoxetine (Prozac), fluvoxamine (Luvox), and sertraline (Zoloft).
- Deep Brain Stimulation (DBS): This is a neurosurgical procedure that involves implanting a device that sends electrical signals to specific areas of the brain. DBS is typically only used for severe cases of OCD that have not responded to other forms of treatment.
- Transcranial Magnetic Stimulation (TMS): TMS is a non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain. It’s used when standard treatments haven’t been effective.
- Self-Care/Lifestyle changes: Regular exercise, a healthy diet, adequate sleep, and reducing caffeine and alcohol can also help manage symptoms of OCD.
- Support groups: These can be incredibly beneficial for individuals with OCD. They offer a safe space to share experiences, advice, and coping strategies.
- Mindfulness and Relaxation Techniques: Techniques such as meditation, yoga, and progressive muscle relaxation can help manage stress and anxiety, potentially reducing the intensity of OCD symptoms.
The research received funding from the Wellcome Trust and is published in the journal Nature Communications.
South West News Service writer James Gamble contributed to this report.

