IRVINE, Calif. — All of the brain-related troubles a case of COVID-19 can cause a patient make it much more likely they’ll deal with Alzheimer’s disease later in life. That’s according to a review of neurological symptoms connected to COVID by a team at the University of California-Irvine. Issues like brain fog, headaches, and lapses in concentration have become common complaints among those suffering from a COVID infection. Now, researchers say their impact is also driving what eventually leads to Alzheimer’s — the most common form of dementia.
In the Journal of Neurochemistry, the team highlights potential links between these two conditions. Their findings note that old age is one of the biggest contributing factors for both the onset of dementia and contracting COVID-19. Now, it appears both diseases boost the effects of the other — working together to damage brain health.
“I believe over the next several years, emerging evidence will further support a link between microbial infection and neurodegenerative diseases,” says corresponding author Thomas Lane, PhD, of UC Irvine, in a media release. “With regards to AD, our laboratory is now infecting different strains of transgenic AD mice with both murine (mouse) coronaviruses as well as murine-adapted SARS-CoV-2 to assess influences on AD neuropathology.”
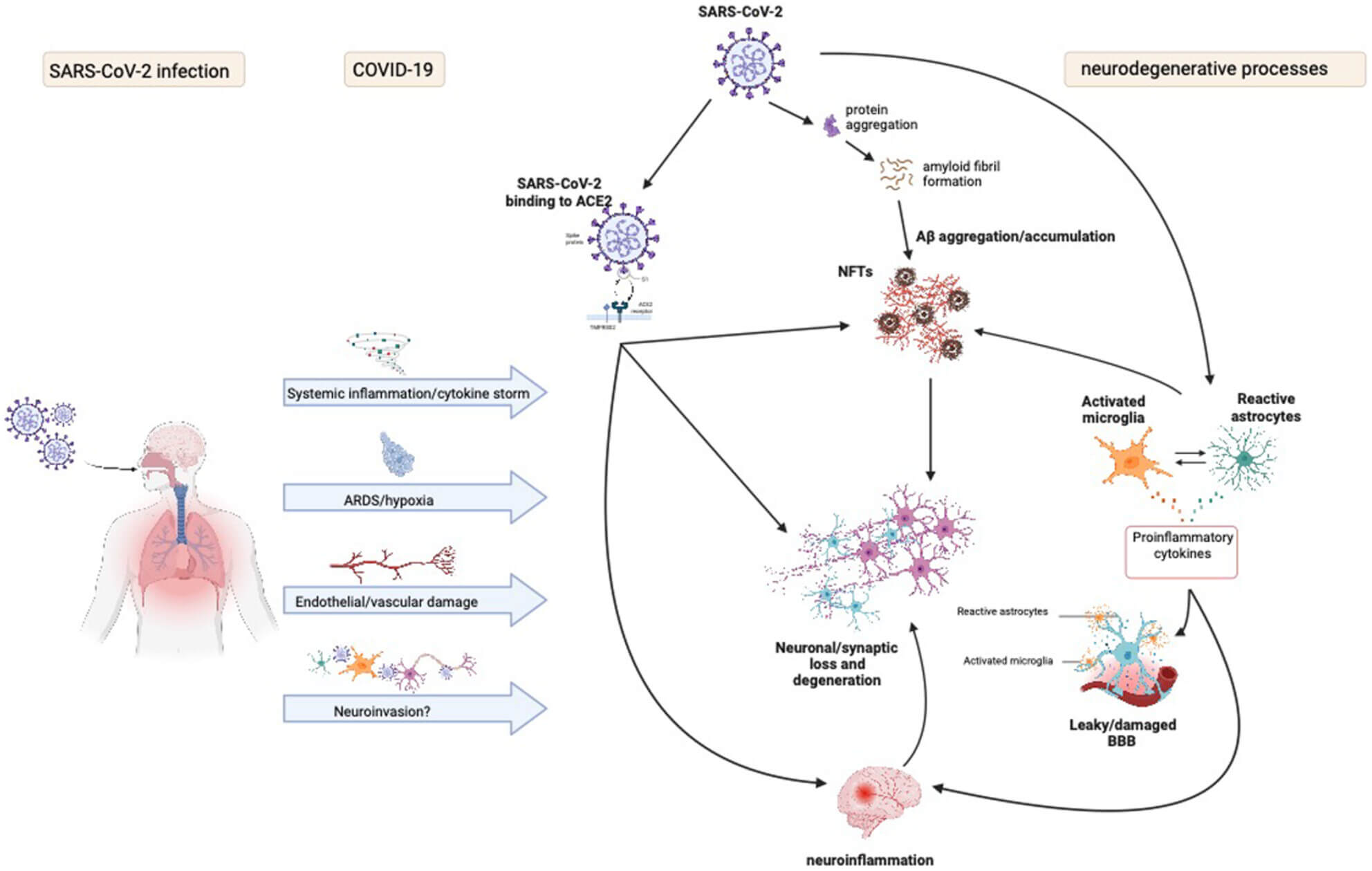
Brain inflammation of COVID-19 looks eerily similar to Alzheimer’s
This isn’t the first study to tie the coronavirus and Alzheimer’s disease together. In 2021, researchers at Stanford Medicine discovered “unmistakable signs” of inflammation and damaged brain circuits among patients who died during the pandemic. What’s even more troubling is this inflammation appears to be very similar to what doctors see in patients who have Alzheimer’s disease and other neurodegenerative diseases.
Stanford’s Dr. Tony Wyss-Coray noted that one-third of hospitalized coronavirus patients report symptoms including fuzzy thinking, forgetfulness, difficulty concentrating, and depression. These problems are also typical in long COVID cases, where patients continue to have side-effects weeks and months after recovering from the virus.
“Viral infection appears to trigger inflammatory responses throughout the body that may cause inflammatory signaling across the blood-brain barrier, which in turn could trip off neuroinflammation in the brain,” Wyss-Coray reported at the time.
You might also be interested in:
- Best Brain Supplements: Top 5 Cognition Boosters Most Recommended By Experts
- These 15 foods in an anti-inflammatory diet could treat long COVID
- COVID-19 increases risk of developing Alzheimer’s in older adults within one year by 80%

The chicom Christmas present that keeps on giving!
But are you a *certified* Facebook scientist??