ST. LOUIS — An extraordinary genetic discovery involving a family from Colombia could pave the way to the end of Alzheimer’s disease. For generations, this particular family has been plagued by the neurodegenerative disease, but one member has remarkably avoided its grip, offering a glimmer of hope for others.
Researchers at Washington University School of Medicine in St. Louis have shed light on a rare genetic mutation known as the Christchurch mutation, found in the APOE gene. This mutation appears to break the link between the early and late phases of Alzheimer’s disease, potentially offering a new approach to preventing dementia.
“Any protective factor is very interesting, because it gives us new clues to how the disease works,” says study senior author Dr. David M. Holtzman, the Barbara Burton and Reuben M. Morriss III Distinguished Professor of Neurology, in a university release.
“As people get older, many begin to develop some amyloid accumulation in their brains. Initially, they remain cognitively normal. However, after many years the amyloid deposition begins to lead to the accumulation of the tau protein. When this happens, cognitive impairment soon ensues. If we can find a way to mimic the effects of the APOE Christchurch mutation, we may be able to stop people who already are on the path to Alzheimer’s dementia from continuing down that path.”
Alzheimer’s takes roughly 3 decades to develop
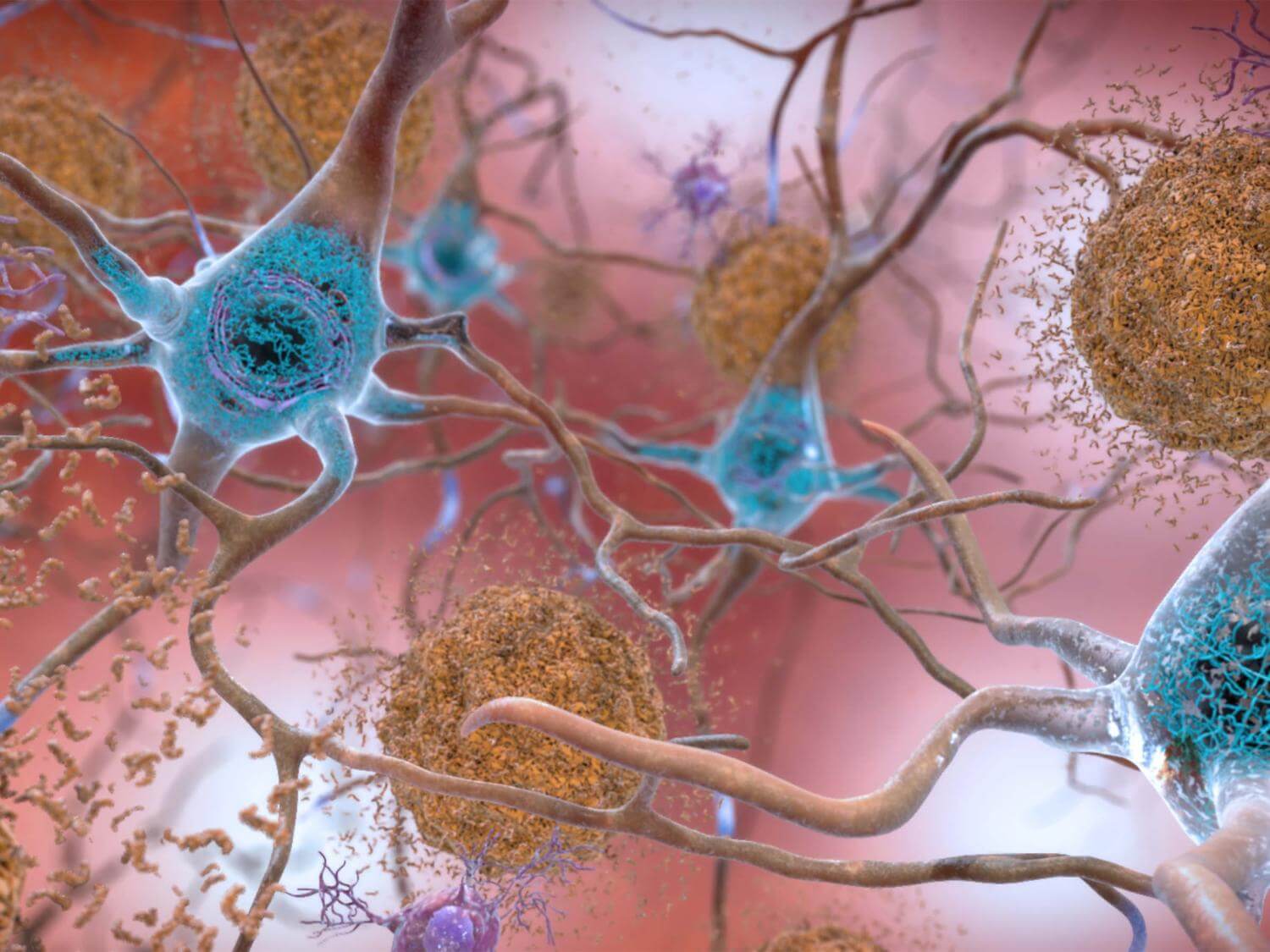
Alzheimer’s typically develops over approximately 30 years, with the initial two decades being symptom-free. During this time, a protein called amyloid beta accumulates in the brain without causing harm. When amyloid levels reach a critical point, phase two begins, involving various destructive processes, including the formation of tangles by a protein called tau, slowing brain metabolism, brain shrinkage, and cognitive decline. This pattern is consistent in both genetic and non-genetic forms of Alzheimer’s.
The Colombian family studied carries a mutation in a gene called presenilin-1, causing excessive amyloid buildup in their brains from their 20s. This rapid amyloid accumulation leads to cognitive decline in middle age. An exceptional case within the family is a woman who, despite having more amyloid in her brain in her 70s than her relatives had in their 40s, displayed minimal signs of brain injury and cognitive impairment.
“One of the biggest unanswered questions in the Alzheimer’s field is why amyloid accumulation leads to tau pathology,” notes Dr. Holtzman. “This woman was very, very unusual in that she had amyloid pathology but not much tau pathology and only very mild cognitive symptoms that came on late. This suggested to us that she might hold clues to this link between amyloid and tau.”
The 2019 study revealed that this woman also carried the Christchurch mutation in both copies of her APOE gene, another gene linked to Alzheimer’s disease. However, with only one person known to possess this unique combination of genetic mutations, there was insufficient data to confirm that the Christchurch mutation was responsible for her resistance to Alzheimer’s.
To address this question, Dr. Holtzman and study first author Yun Chen turned to genetically modified mice. They introduced the Christchurch mutation into mice predisposed to overproduce amyloid and injected human tau into their brains. In normal circumstances, this would initiate a pathological process where tau aggregates at the injection site and spreads throughout the brain. However, in mice with the Christchurch mutation, minor tau pathology developed despite extensive amyloid plaques.
The researchers discovered that the key difference lay in the activity levels of microglia, the brain’s waste-disposal cells. In mice with the APOE Christchurch mutation, microglia surrounding amyloid plaques were highly effective at consuming and disposing of tau aggregates.
“These microglia are taking up the tau and degrading it before tau pathology can spread effectively to the next cell,” explains Dr. Holtzman. “That blocked much of the downstream process; without tau pathology, you don’t get neurodegeneration, atrophy and cognitive problems. If we can mimic the effect that the mutation is having, we may be able to render amyloid accumulation harmless, or at least much less harmful, and protect people from developing cognitive impairments.”
This innovative research offers newfound hope in the fight against Alzheimer’s disease, providing a potential avenue for the development of preventive measures to halt or mitigate its devastating effects. While more research is needed, the Christchurch mutation has opened a promising door for scientists in their quest to understand and combat this debilitating disease.
The study is published in the journal Cell.
You might also be interested in:
- Nanoparticles may help untangle brain blockages caused by Alzheimer’s disease
- Carrying Alzheimer’s genes may also increase your risk for developing epilepsy
- A healthy lifestyle staves off dementia in old age — regardless of your genetic risk

