SOLNA, Sweden — A startling new study from Swedish researchers shows that having a high metabolism could be an early warning sign of Alzheimer’s disease onset later in life. Scientists from the Karolinska Institutet were able to identify an early metabolic shift in the brain’s hippocampus as a potential indicator of the deadly neurodegenerative disease.
This discovery opens doors for new strategies in early intervention for Alzheimer’s, which affects approximately 500,000 people in the United States every year.
Alzheimer’s disease is the most common form of dementia, and its onset is often insidious, occurring years before noticeable symptoms manifest. Researchers found that an increase in metabolism within the brain’s cellular powerhouses, known as mitochondria, is an early sign of the disease.
To investigate this phenomenon, researchers used mouse models that develop Alzheimer’s pathology in a manner similar to humans. They observed an increase in metabolic activity in young mice, which was followed by synaptic changes linked to disruptions in the cellular recycling system, known as autophagy — a process recognized with the Nobel Prize in Physiology or Medicine in 2016.
Over time, the metabolic activity in the brains of Alzheimer’s patients typically declines, contributing to the deterioration of synapses. This decline was also evident in older mice with the disease.
“The disease starts to develop 20 years before the onset of symptoms, so it’s important to detect it early – especially given the retardant medicines that are starting to arrive,” says Dr. Per Nilsson, associate professor at Karolinska Institutet’s Department of Neurobiology, Care Sciences and Society, in a university release. “Metabolic changes can be a diagnostic factor in this.”
“Interestingly, changes in metabolism can be seen before any of the characteristic insoluble plaques have accumulated in the brain,” adds Maria Ankarcrona, professor Karolinska Institutet’s Department of Neurobiology, Care Sciences and Society. “The different energy balance tallies with what we’ve seen in images of the Alzheimer brain, but we’ve now detected these changes at an earlier stage.”
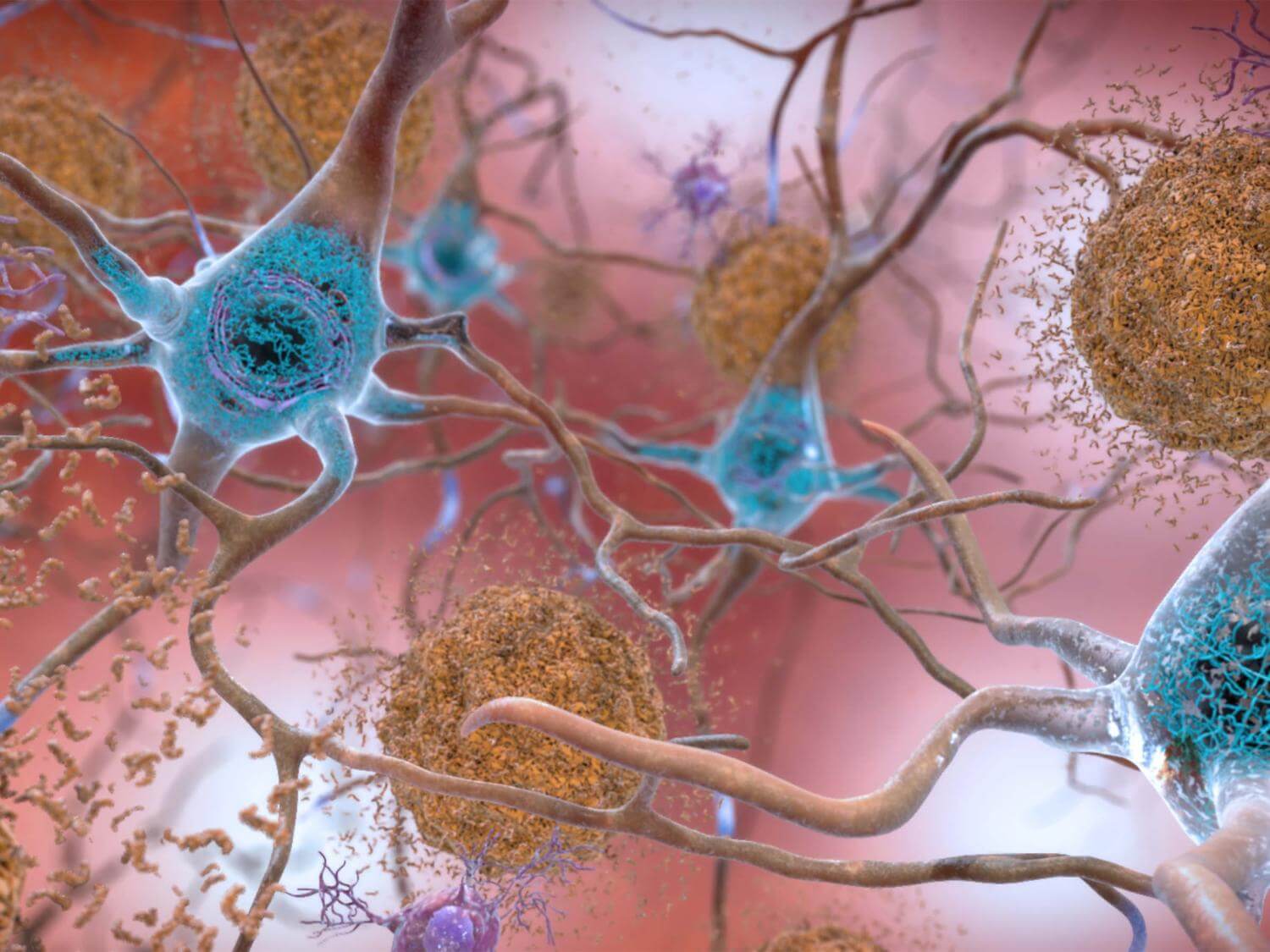
The study focused on the hippocampus, a brain region crucial for short-term memory and one of the earliest areas affected in Alzheimer’s patients. By using RNA sequencing to identify active genes during various disease stages, the researchers pinpointed an increase in mitochondrial metabolism as an early marker of Alzheimer’s.
To investigate synaptic changes, the team employed electron microscopy and other techniques. They found that autophagosomes, vesicles responsible for breaking down spent proteins and their components, had accumulated in the synapses. This buildup disrupted access to functional proteins, contributing to the disease’s progression.
Researchers plan to delve deeper into the roles of mitochondria and autophagy in Alzheimer’s disease, using mouse models that closely mimic the Alzheimer’s brain.
“These findings highlight the importance of retaining functional mitochondria and normal protein metabolism,” says Dr. Nilsson. “Going forward, we’ll be able to do tests on mice to see if new molecules that stabilize mitochondrial and autophagic function can retard the disease.”
The study is published in the journal Molecular Psychiatry.
You might also be interested in:
- 3 Ways To Improve Your Metabolism — And The 1 Thing You Shouldn’t Be Doing
- Best Brain Supplements: Top 5 Cognition Boosters Most Recommended By Experts
- Number of dementia cases by 2040 could be shockingly higher than estimates predicted
- Fitness crisis? Just 7% of U.S. adults have good cardiometabolic health