WAKO, Japan — A prescription drug for patients dealing with kidney cancer may also be able to repair damaged blood vessels in the brain, according to new research. This could be a potential lifesaver for the approximately 30,000 Americans who experience a ruptured aneurysm each year.
Aneurysms are a bulge in a weak area of a blood vessel, which can result in devastating internal bleeding. Roughly six percent of the U.S. population have this condition in the brain, often referred to as a “silent killer” due to its largely symptomless nature, causing no significant daily problems. These brain aneurysms can usually only be detected through medical imaging scans.
“Unruptured intracranial aneurysms are usually detected by Magnetic Resonance Angiography or Computed Tomography Angiography during health checkups. If these tests are not available, then aneurysms are undetectable until they burst,” says lead author Dr. Hirofumi Nakatomi from the of the RIKEN Center for Brain Science in Japan.
A brain aneurysm can rupture without warning. In 50 percent of cases, this results in almost instantaneous death. Many of the survivors are left with permanent brain damage. Symptoms can range from severe headaches and vision issues to a potentially fatal stroke.
Research experiments revealed that these aneurysms are often caused by a gene mutation known as PDGFRB. In studies conducted on mice, however, the anti-tumor medication Sunitinib was found to block this gene’s activity, thereby preventing aneurysm formation. This finding is particularly relevant to intracranial saccular aneurysms (ISAs), the most common type, accounting for over 90 percent of cases. Risk factors for aneurysms include age, high blood pressure, smoking, and alcohol consumption.
“The unexpected finding that greater than 90% of aneurysms had mutations in a common set of 16 genes indicates that somatic mutation could be the major trigger in most cases,” Dr. Nakatomi adds in a media release.
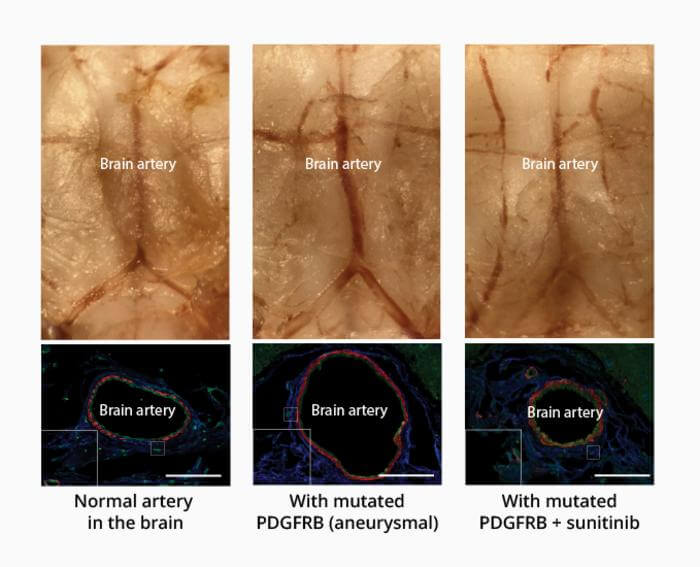
The research team linked the gene variant to increased cell migration and inflammation in cultured cells and found that these effects could be blocked with Sunitinib — which is available to patients under the brand name Sutent. They genetically engineered lab rodents to carry the mutant gene at the base of the brain. After a month, the diameter of the affected artery had doubled, and the artery had become significantly weaker. However, the effect was reversed when the mice were treated with Sunitinib, resulting in normal-sized, strong basilar arteries.
“Establishing the first non-surgical animal model of intracranial aneurysm is in itself an achievement,” Nakatomi explains, “but more importantly, we suppressed artery expansion with a drug, indicating that intracranial aneurysms can be pharmacologically treated.”
More research is necessary to establish whether this treatment can be effective in humans. Perhaps an even greater challenge lies in detecting aneurysms early enough for such treatment. According to Dr. Nakatomi, in Japan, many people undergo these types of tests as part of their annual health check-up, making the development of drug treatments especially beneficial.
Currently, surgeons repair aneurysms by inserting tiny metal coils or a mesh ball known as a cerebral aneurysm embolization device, or sometimes both. These implants work by blocking blood flow to the aneurysm, effectively sealing it off to prevent rupture. They are usually placed via a catheter inserted into a vein in the thigh or wrist and then threaded through to the brain.
The study is published in the journal Science Translational Medicine.
You might also be interested in:
- Ultrasonic ‘tornado’ can break down blood clots in the brain
- Following a plant-based diet lowers risk of blood clots in the brain
- Eye doctor saves girl’s life after routine test discovers potentially fatal brain condition
South West News Service writer Mark Waghorn contributed to this report.