SYDNEY, Australia — Animal testing is traditionally the first step when testing drugs and how they might potentially affect humans. However, there are a number of financial and ethical reasons to cut down on the number of animal experiments. One replacement is creating mini-organs to simulate the real thing. Researchers in Australia are looking at a new approach for creating advanced 3D lung structures — all starting in a single petri dish.
According to the authors, lung models could shorten drug development times. Currently, it takes about 10 to 15 years to test a drug before it actually reaches the market.
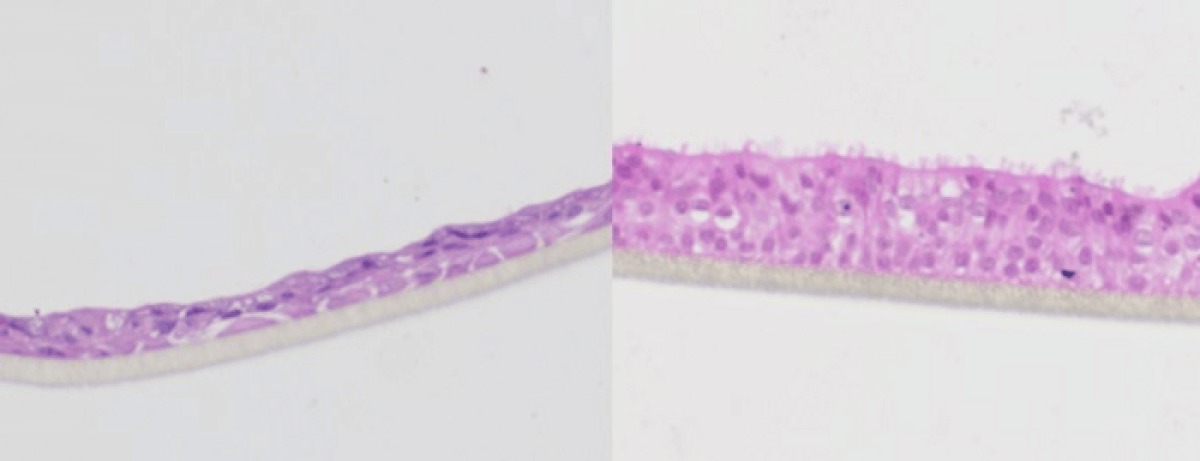
Scientists created two lab-made lung models from human primary cells. The first one resembles a healthy lung to test the safety of a new drug. The second mimics phase 2 trials, where researchers test new drugs on a diseased lung. In this scenario, the unhealthy lung resembled the ones seen in people with chronic obstructive pulmonary disease (COPD).
“We take cells directly from patients and then build them in layers as they exist inside the body. So, first you have the epithelial cells, then you have the fibroblasts—we are literally creating a mimic organ that is very much like actual human lungs,” says Wojciech Chrzanowski, a professor of nanomedicine at the University of Sydney and co-author of the study, in a media release.
“With a traditional cell culture, you put cells into a Petri dish and culture them in static conditions, which is far from what happens in a human body. What we are doing is creating environmental conditions similar to those which exist in the human body,” explains lead study author Huyen Phan, a researcher at the University of Sydney.
To maintain similar environmental conditions as a human lung, the researchers kept the air on one side and a liquid interface at the bottom along with microcirculation that would resemble blood circulation.
“These two elements combined help emulate the conditions of a human lung, making them more accurate,” the team explains.
Looking beyond drug testing, the lung models have the potential to help with creating personalized medications for people. For example, if you wanted to test a range of reactions in a lung, you can take a sample of cells from a person and create a lung that most resembles theirs. The mini-organs could also help with testing the danger of air-borne pollutants in areas with high levels of air pollution or forest fires.
“They accelerate the process of discovery, they shorten the process of getting to clinics, but also substantially increase our confidence in the molecules we create before we go to clinical trials,” says Chrzanowski.
The study is published on the preprint server of Biomaterials Research, meaning the findings are still awaiting peer review from other scientists.
You might also be interested in:
- Lab-grown ‘mini-brains’ open door to better treatments for dementia, ALS
- Cure for blindness on the horizon? Lab-grown eye cells successfully ‘connect’ to retina
- Inhalable powder protects lungs from flu, other respiratory viruses