PHILADELPHIA — A promising new vaccine is showing the potential to treat high-risk multiple myeloma, a chronic and incurable form of cancer. Scientists from the Moffitt Cancer Center say the dendritic cell vaccine could empower patients’ immune systems to push the cancer into remission and potentially prevent its return.
The study revolved around a dendritic cell vaccine that specifically targets a protein named survivin. This vaccine was tested on 13 patients with multiple myeloma through a phase I clinical trial. Each patient took the vaccine before and after undergoing an autologous stem cell transplant (ASCT) – a common treatment method where patients’ own stem cells help replace diseased bone marrow.
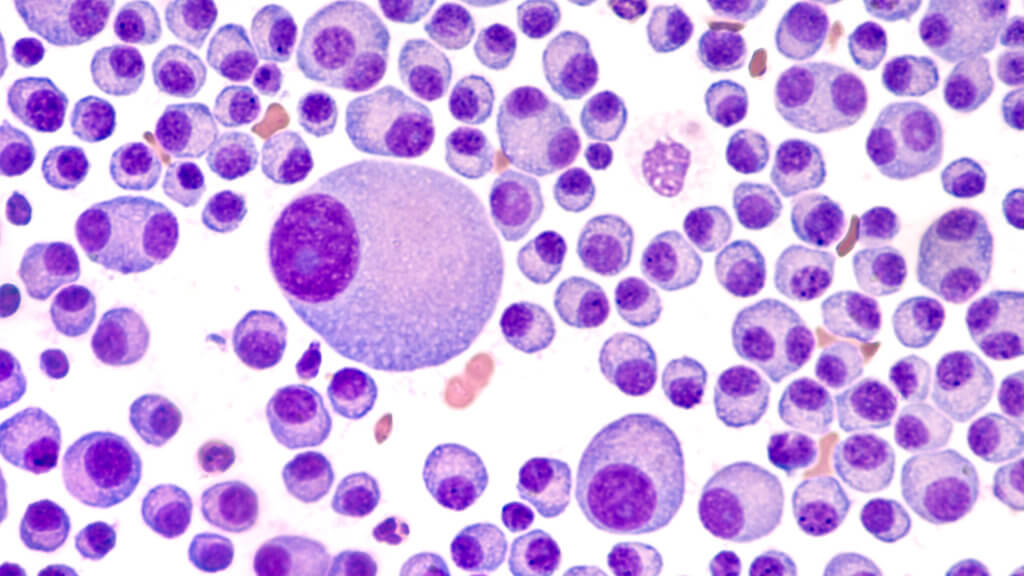
Dendritic cells are crucial to our immune systems. They absorb foreign proteins, fragment them, and introduce these fragments to other immune cells to activate a defense mechanism. For the study, scientists manipulated patients’ dendritic cells to target the survivin protein, aiming to incite an immune response against it.
“High expression of survivin at diagnosis is associated with poor outcomes,” says study senior author Dr. Frederick Locke, chair of the Blood and Marrow Transplant and Cellular Immunotherapy Department at Moffitt Cancer Center Locke, in a media release. “Therefore, we hypothesized that by targeting this protein, we could induce an immune response in patients who have the most aggressive disease and potentially keep them in remission for a longer period of time.”
Dr. Locke and his team further ensured the dendritic cells exposed the entire survivin protein, albeit with a slight mutation to enhance safety while maintaining its immune-response triggering properties.
The findings indicated that the vaccine, combined with ASCT, had a favorable safety profile with only minor side effects. Additionally, the vaccine was able to prompt a survivin-specific immune reaction. After vaccination and ASCT, 85 percent of the patients exhibited either a T-cell response or an antibody response against survivin.
Out of the participating patients, seven showcased enhanced clinical outcomes 90 days post-transplant, all of whom had displayed survivin-specific immune responses. After an average monitoring period of 4.2 years, six of these seven patients continued to be disease-free.
“These results compared very favorably to historical data suggesting the four-year progression-free survival of this patient population to be approximately 50 percent,” says Dr. Locke.
However, Dr. Locke stresses the need for more extensive studies to verify these promising findings and to explore the potential benefits of administering the vaccine earlier in the disease’s progression.
There were some study limitations, though, such as the unique patient demographic that doesn’t usually feature in clinical trials and the rapid evolution of myeloma treatments. Another concern was the limited sample size, which meant that researchers couldn’t conclusively determine if the immune responses triggered by the vaccine were directly combating the patients’ myeloma cells.
The study is published in the journal Clinical Cancer Research.
You might also be interested in:
- Off-the-shelf immune drug may treat aggressive multiple myeloma
- New vaccine uses live tumor cells to kill and prevent brain cancer
- Cancer cure could be uncovered from patient who survived a dozen tumors

