CAMBRIDGE, Mass. — A personalized 3D-printed artificial heart beats just like the real thing — enabling doctors to tailor implants for individual patients. Scientists at MIT, who are creating the new technology, say no two organs are alike, with size and shape varying from one person to the next. The robotic device is a soft and flexible replica which can mimic the organ’s blood-pumping ability.
“All hearts are different,” says Luca Rosalia, a graduate student in the MIT-Harvard Program in Health Sciences and Technology, in a media release.
“There are massive variations, especially when patients are sick. The advantage of our system is that we can recreate not just the form of a patient’s heart, but also its function in both physiology and disease.”
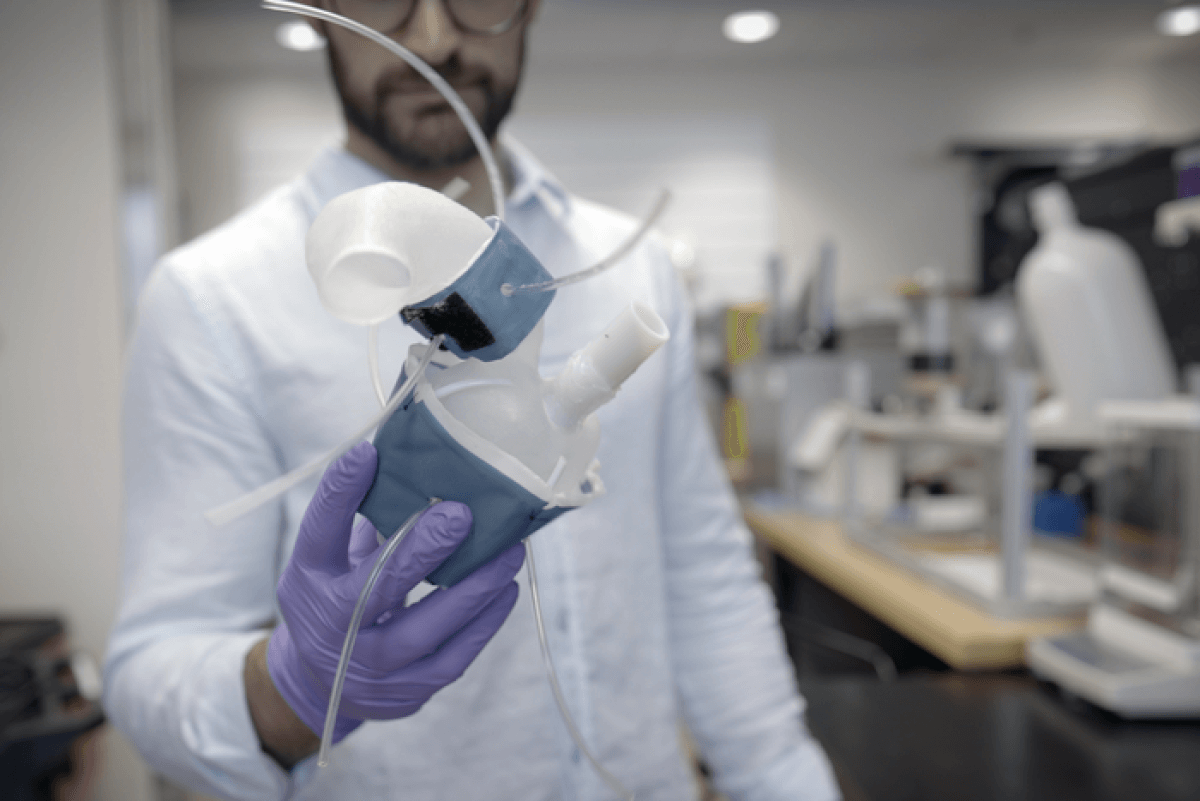
Medical images are converted into a three-dimensional computer model which is 3D printed using a polymer-based ink. Once scientists print and cure the device, it can squeeze and stretch similar to a real beating heart. The resulting shell is an exact copy of the actual organ’s measurements.
The approach can also print out the aorta — the major artery that carries blood out of the heart to the rest of the body. Fabricated sleeves similar to blood pressure cuffs wrap around them to simulate pumping. The underside resembles precisely patterned bubble wrap.
Connecting it to a pneumatic system tunes outflowing air to rhythmically inflate the bubbles and contract the heart. Inflating a separate sleeve surrounding a printed aorta constricts the vessel. This can mimic a condition called aortic stenosis, where the valve narrows and causes the heart to work harder to force blood through the body.
3D-printed hearts could become perfect test models for doctors
A common treatment is surgically implanting a synthetic valve designed to widen it. In the future, doctors could 3D print a patient’s heart and aorta then implant a variety of devices to see which results in the best function and fit. The heart replicas could also help research labs and the medical device companies, serving as realistic platforms for testing therapies for various types of heart conditions.
“There is a lot of interest in the medical field in using 3D-printing technology to accurately recreate patient anatomy for use in preprocedural planning and training,” notes co-author Dr. Sophie Wang, a vascular surgeon at Beth Israel Deaconess Medical Center.
The method allows scientists to find a patient’s exact fit
The study used medical scans of 15 patients diagnosed with aortic stenosis. The team converted images into a three-dimensional computer model of their left ventricle (the main pumping chamber) and the aorta. For each model heart, the researchers could accurately recreate the same heart-pumping pressures and flows that were previously measured in each respective patient.
“Being able to match the patients’ flows and pressures was very encouraging,” says co-author Dr. Ellen Roche of Massachusetts General Hospital. “We’re not only printing the heart’s anatomy, but also replicating its mechanics and physiology. That’s the part that we get excited about.”
When the team implanted valves as they pumped, the researchers observed that they produced similar improved flows as seen in patients following their procedures.
“Patients would get their imaging done, which they do anyway, and we would use that to make this system, ideally within the day,” says co-author Dr. Christopher Nguyen of the Cleveland Clinic. “Once it’s up and running, clinicians could test different valve types and sizes and see which works best, then use that to implant.”
Ultimately, the patient-specific replicas could help develop and identify ideal treatments for individuals with unique and challenging cardiac geometries.
“Designing inclusively for a large range of anatomies, and testing interventions across this range, may increase the addressable target population for minimally invasive procedures,” Roche concludes.
The study is published in the journal Science Robotics.
South West News Service writer Mark Waghorn contributed to this report.