No bigger than a credit card, the placenta-on-a-chip could create personalized treatments for pregnant women and their babies.
AMES, Iowa — Our understanding of prenatal health could reach new heights thanks to the development of a “placenta-on-a-chip.” Developed by Nicole Hashemi, an associate professor of mechanical engineering at Iowa State University, and her research team, this innovative technology has the potential to advance personalized medicine and improve the safety of prenatal treatments.
The placenta is a fascinating organ that plays a crucial role in fetal development. It acts as a barrier between the mother’s and the fetus’s blood supply, allowing the exchange of nutrients, oxygen, and waste products while protecting the fetus from harmful substances. However, studying the placenta in real time has been a challenge for researchers, as it is difficult to observe without invasive procedures.
This is where the placenta-on-a-chip comes in. No bigger than a credit card, the device consists of two microchannels, just millionths of a meter wide and high, separated by a porous membrane. One channel represents the maternal blood flow, while the other represents the fetal blood flow. The membrane between the channels mimics the placental barrier, especially when it is lined with endothelial or barrier-forming cells.
By pumping fluids through the model, researchers can test how various substances, such as medicines and nutrients, cross the placental barrier from mother to fetus and vice versa. This technology could help scientists better understand the complex processes that occur within the placenta and how they affect fetal development.
Hashemi and her team have been working on this project since 2015, and their persistence is finally paying off. With a recent National Science Foundation (NSF) Mid-Career Advancement grant, the researchers can now explore new developments in sensing, personalized medicine, and commercialization.
“We’re still working on our ‘placenta-on-a-chip’ project,” Hashemi says in a university release. “With this grant we’re trying to design sensing platforms that can be integrated to the model.”
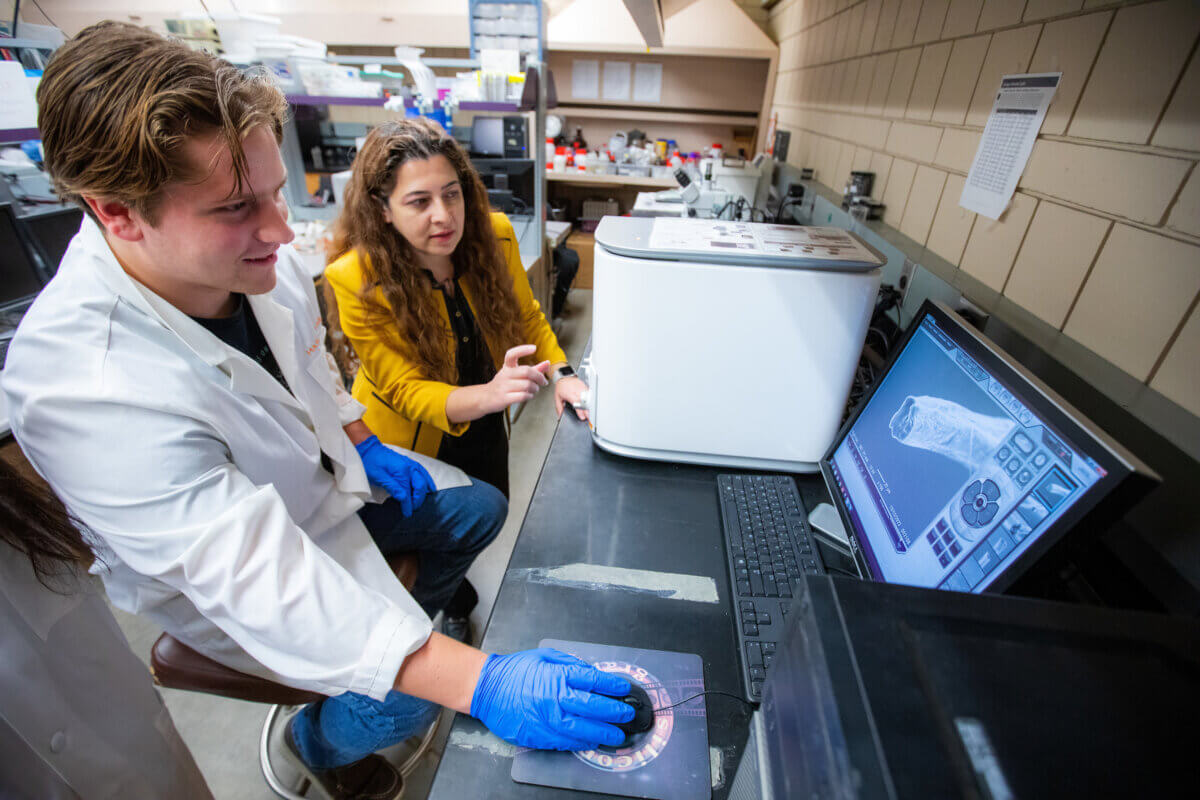
One of the sensing platforms will use ions – atoms and molecules with different numbers of electrons, creating positive or negative charges – to sense how cells react to mechanical forces or chemical stressors. The other platform will employ “hyperspectral” imaging technology, which records a broad spectrum of light, to sense how cells respond to chemical stressors. This technology is being incorporated through a collaboration with Juan Santiago, a professor of mechanical engineering at Stanford University.
In addition to these sensing platforms, Hashemi hopes to use a patient’s own cells in the placenta-on-a-chip model to advance personalized medicine. This could lead to more accurate testing for the transport rate of specific compounds and setting safe exposure levels for individual patients.
The placenta-on-a-chip has already demonstrated several potential applications. In one published study, the researchers tracked caffeine transport across the placental barrier. They also have a research partnership with the University of Nebraska College of Medicine to measure the movement of nanomedicines through the placental barrier.
“There are a lot of ideas about how to use this platform technology,” Hashemi says.
As part of the NSF grant, Hashemi’s graduate students will also explore opportunities to commercialize this technology. This could lead to the development of a startup or industry partnerships, bringing the placenta-on-a-chip closer to real-world applications for mothers-to-be.
By better understanding how substances cross the placental barrier, scientists can develop safer and more effective treatments for pregnant women and their unborn children. This could include more targeted drug delivery systems, improved prenatal nutrition, and better monitoring of fetal health.
“The goal is to have a new prototype by the end of the grant’s third year,” Hashemi concludes. “But we’ll be spending a lot of time on the basic science to develop these two new sensing systems. We hope to ultimately contribute to solving the critical challenges related to human health, in this case for both women and their children.”
StudyFinds Editor-in-Chief Steve Fink contributed to this report.
