CHICAGO — Artificial Intelligence (AI) might play a vital role in identifying non-smokers who are at risk of developing lung cancer, according to new research. Scientists employed an AI model to assess the risk of lung cancer in non-smokers by analyzing a single chest X-ray. Their findings show that this model accurately pinpointed about 30 percent of the nearly 17,500 patients involved as having a 2.1 times higher risk of developing lung cancer.
The research team hails the new project as being able to identify at-risk patients of the world’s deadliest cancer, as it is currently difficult to predict this risk in those who do not or have rarely smoked.
Lung cancer is the leading cause of cancer death worldwide and accounts for nearly half of all new cancer cases in the United States, including breast, bronchus, prostate, and colorectal cancers. The American Cancer Society estimates about 238,340 new lung cancer cases and approximately 127,000 deaths from the disease this year. Notably, 10 to 20 percent of lung cancers occur in individuals who have never smoked or have a minimal smoking history.
Despite this, current screening guidelines often exclude these groups. The United States Preventive Services Task Force (USPSTF) recommends lung cancer screening primarily for adults between 50 and 80 with a significant smoking history, typically not covering those who have never smoked or have smoked very little.
“Current Medicare and USPSTF guidelines recommend lung cancer screening CT only for individuals with a substantial smoking history,” says Anika Walia, the study’s lead author, and researcher at the Cardiovascular Imaging Research Center (CIRC) at Massachusetts General Hospital (MGH) and Harvard Medical School, in a media release. “However, lung cancer is increasingly common in never-smokers and often presents at an advanced stage.”
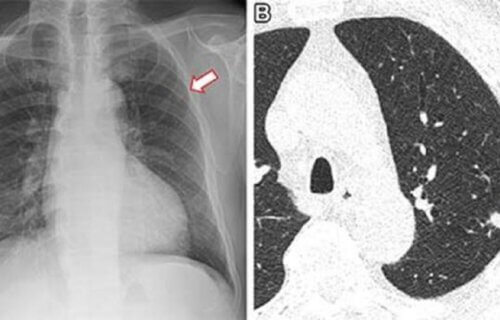
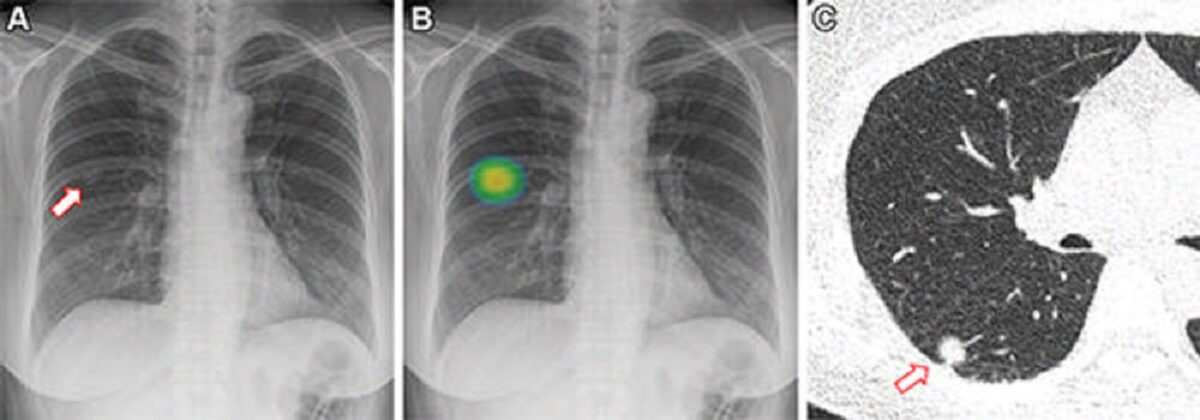
To address this, CIRC researchers developed a deep learning AI model, dubbed CXR-Lung-Risk. This model can assess lung cancer risk in non-smokers by analyzing chest X-rays. Deep learning, a sophisticated AI technique, scans X-ray images for patterns indicative of disease.
“A significant advantage of our method is that it only requires a single chest X-ray, a test that is both highly common and easily accessible,” Walia highlights.
The model was trained using nearly 150,000 chest X-rays from the Prostate, Lung, Colorectal, and Ovarian (PLCO) cancer screening trial, encompassing both smokers and never-smokers. It was then validated in a separate group of never-smokers undergoing routine outpatient chest X-rays.
The primary measure was the six-year incidence of lung cancer, with patients categorized into low, moderate, and high-risk groups. In a sample of 17,407 patients, 28 percent were identified as high-risk, with 2.9 percent later diagnosed with lung cancer — exceeding the 1.3 percent six-year risk threshold for recommended screening.
“Even after adjusting for various factors, the high-risk group showed a 2.1 times greater likelihood of developing lung cancer compared to the low-risk group,” Walia adds.
The researcher sees this AI tool as a pathway for opportunistic screening of non-smokers at high risk, utilizing existing chest X-rays in medical records.
“With declining smoking rates, it’s increasingly important to find methods for early lung cancer detection in non-smokers,” concludes Dr. Michael Lu, the study’s senior author and director of artificial intelligence at CIRC at MGH.
The study was presented at the Radiological Society of North America’s (RSNA) annual meeting in Chicago.
You might also be interested in:
- AI screening tool twice as effective at discovering lung cancer before it’s too late
- Scientists uncover how air pollution causes lung cancer in non-smokers
- Healthiest Cities In America: Top 5 Places For Wellness, According To Experts
South West News Service writer James Gamble contributed to this report.